Lena was the person who could name every “healthy” snack aisle brand. Almond flour crackers, low-calorie wraps, protein cereal. She tracked, she weighed, she detoxed, she tried to outsmart her body. And every January she got the same result: a few pounds down, then a hard stop—followed by rebound.
By 2025, the weight wasn’t the only problem. She was tired in the morning, ravenous at 4 PM, and strangely “softer” even when the scale dipped. When GLP‑1 medications became mainstream, she almost booked a telehealth appointment—until a clinician asked one question that changed everything: “How much muscle do you actually have?”
The modern weight-loss trap is not overeating. It’s under-muscling, under-sleeping, and over-stressing in a food environment designed to spike cravings.
Key takeaways
- Stubborn fat loss is often a body composition problem, not a motivation problem—low lean mass makes your “metabolic engine” smaller.
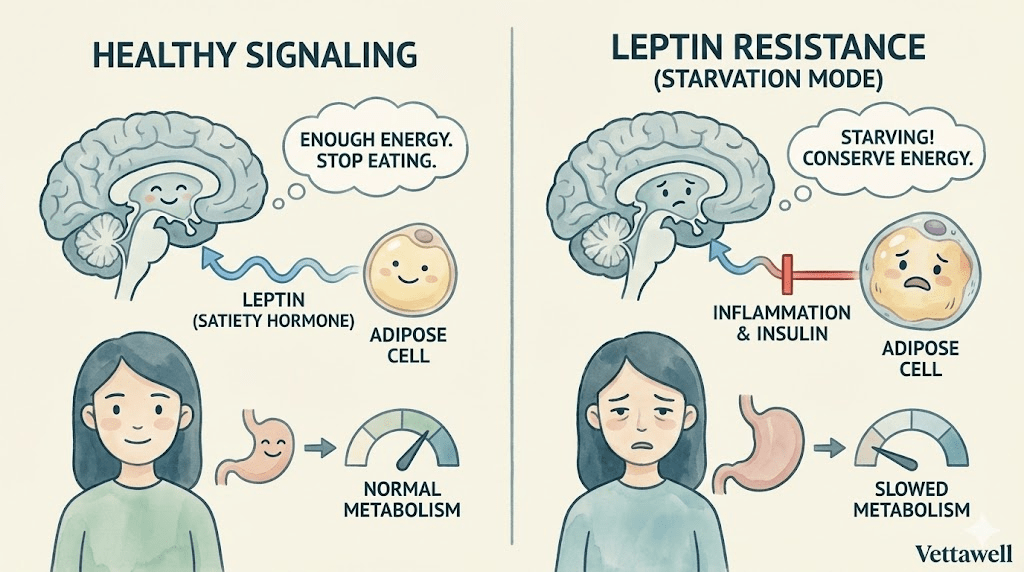
- Unstable blood sugar can create a daily cycle of cravings → restriction → overeating without you realizing it.
- In the post‑GLP‑1 era, “successful weight loss” means fat loss with muscle preserved, not simply a lighter scale number.
- A sustainable plan starts with three non‑negotiables: a protein floor, daily steps (especially after meals), and strength training.
- If you don’t fix recovery (sleep, stress, and meal timing), your body will keep defending the same set point.
Lena’s starting point (and why it looked “fine” on paper)
Lena was 33, working in product management, and had gained about 25–30 pounds over four years of remote work. Her labs were “normal.” Her BMI was in the “overweight” range but not extreme. She exercised more than her friends—spin twice a week, Pilates on weekends, occasional bootcamp.
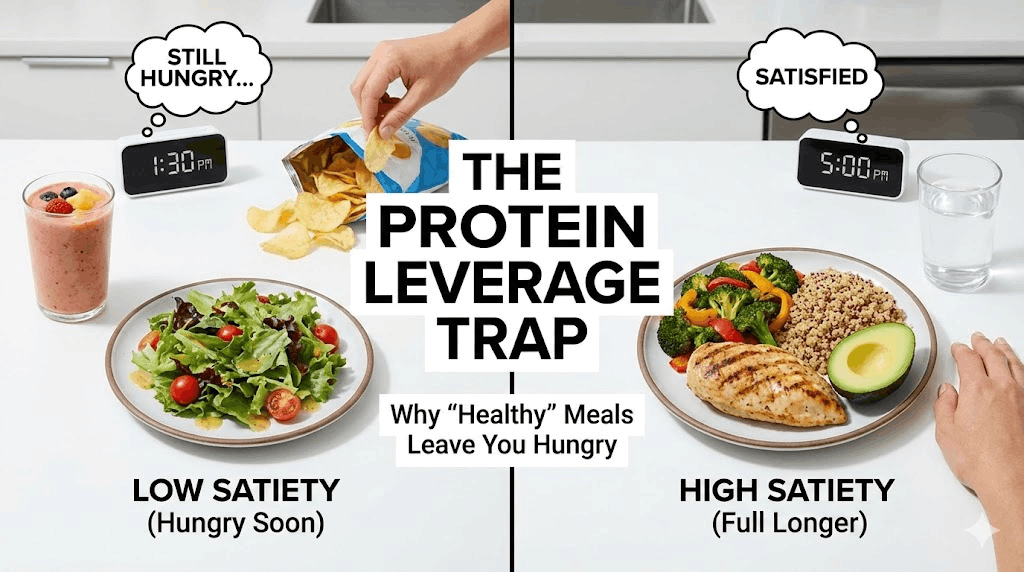
Her diet sounded disciplined: salad lunches, smoothies, “light” dinners. But she had two invisible problems that are extremely common in 2025:
- Problem #1: A small muscle bank. Years of cardio without progressive resistance training meant she didn’t have much lean mass to buffer glucose or keep resting energy expenditure high.
- Problem #2: A glucose rollercoaster disguised as “healthy eating.” Smoothies, granola, wraps, and “fat‑free” snacks kept her insulin high—then crashed her energy and drove evening hunger.
The wake-up call
The moment that broke her wasn’t the scale. It was a photo. At a friend’s birthday, she saw herself in a candid shot from the side—rounded shoulders, a tired face, and a body that looked older than she felt. "I realized I wasn’t just heavier," she said. "I looked inflamed."
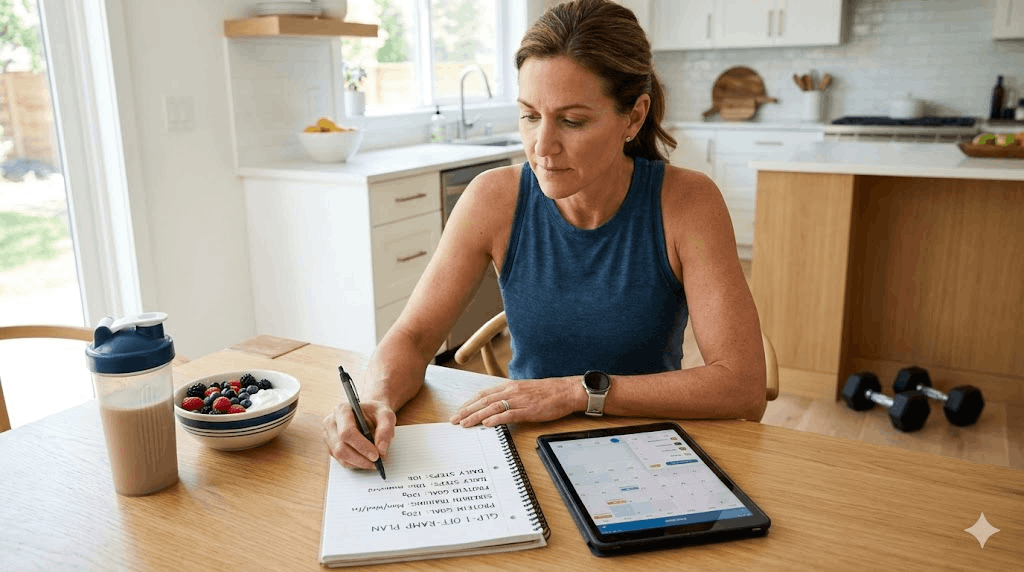
She booked a consultation with a clinician who did something no diet plan had ever done: they measured her composition (waist, strength, and lean mass estimate) and mapped her day like a metabolic timeline.
- You’re not failing. Your strategy is. Your plan is built around eating less, not building capacity.
- Your body is defending energy because it thinks you’re under-fueled and over-threatened. Low sleep + high stress + high-intensity workouts signal scarcity.
- You don’t need a new diet. You need a new order of operations.
You can’t starve a body into calm. You have to train it into stability.
The real culprit: the ‘protein deficit’ + ‘snack economy’ combo
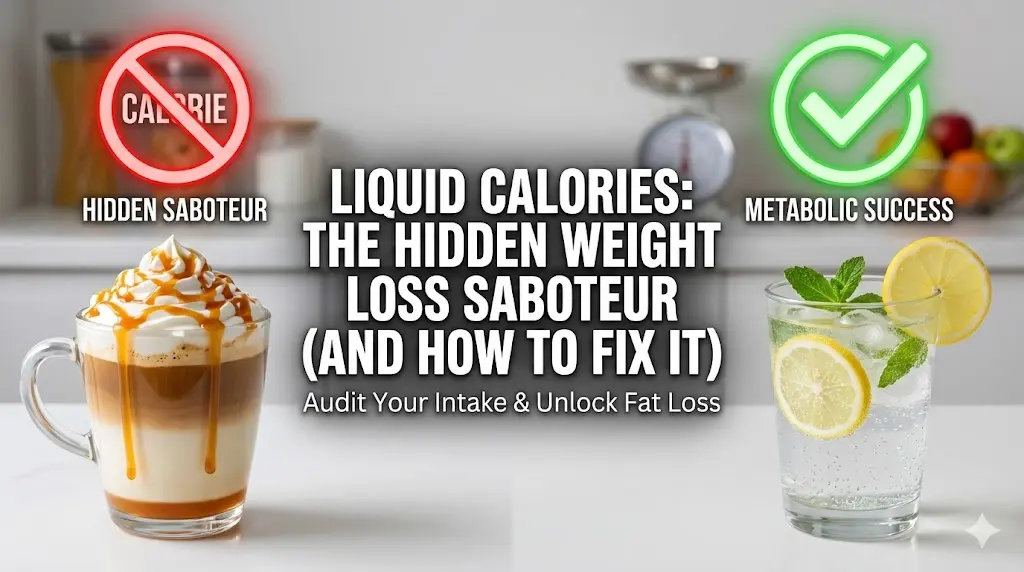
When Lena logged her intake honestly (not aspirationally), her daily protein averaged 55–70g. For her goals, it was low. She also had a pattern that many people don’t count: micro-snacking—a handful here, a latte there, a “healthy bar” at the desk.
This mattered for two reasons:
- Protein is the satiety anchor. Without it, hunger hormones stay loud and cravings become negotiations you lose at night.
- Constant grazing keeps insulin elevated. When insulin stays high all day, fat release from adipose tissue is restricted—so your body asks for more food instead.
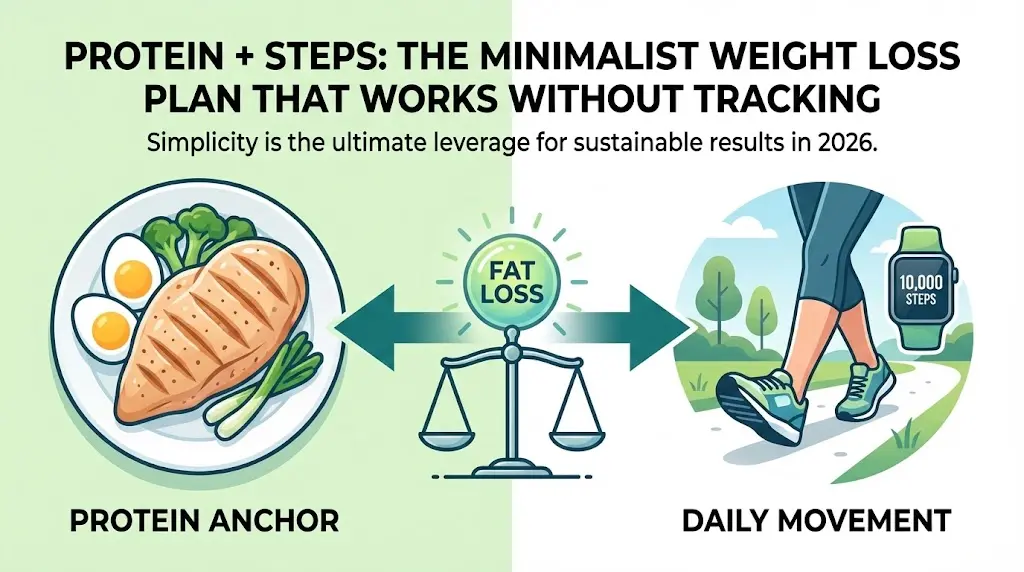
The protocol: 12 weeks to rebuild the engine
Instead of a “diet,” Lena followed a protocol with three levers. The goal was simple: stabilize appetite, protect muscle, and create a mild deficit without feeling punished.
She stopped chasing “perfect meals” and started chasing a number. Her target wasn’t extreme; it was consistent: a protein floor every day.
- Target: 30–40g protein at breakfast, then 25–35g at lunch and dinner (adjust to body size and clinician guidance).
- Rule: If a meal didn’t have a clear protein source, it didn’t count as a meal—it was a snack.
- Shortcut meals: Greek yogurt + berries + nuts; eggs + cottage cheese; chicken salad; tofu stir‑fry; tuna + lentils.
A calorie deficit is fragile. A protein floor is stable. Build the stable thing first.
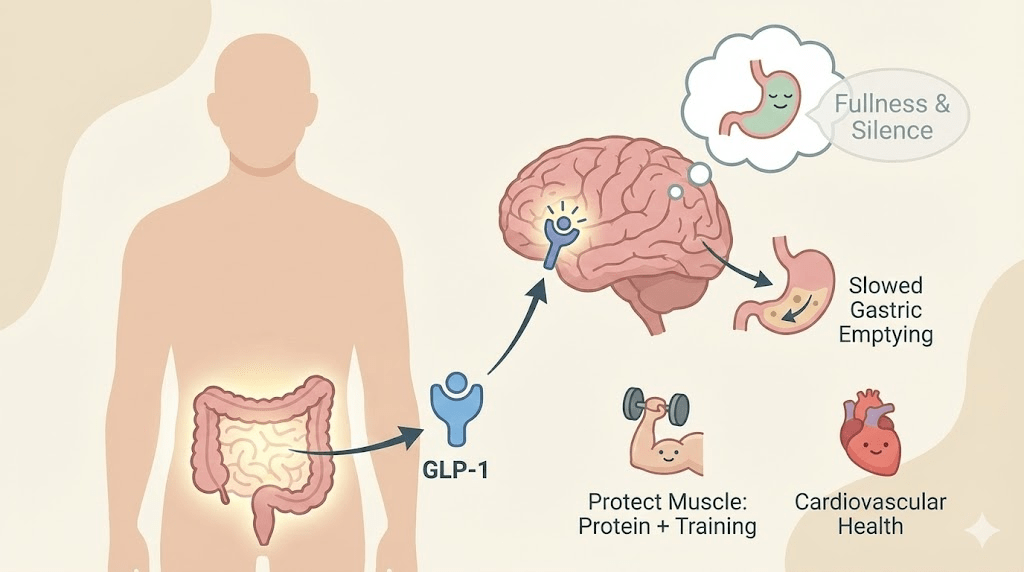
Lena didn’t add more workouts. She added 10 minutes of walking after her two biggest meals. Not speed walking, not “fat burn cardio”—just movement.
- Why it worked: contracting muscles pull glucose out of the bloodstream with less insulin demand, flattening the post‑meal spike.
- Why it was sustainable: it fit into her life—phone calls, podcasts, walking the dog.
- Non‑negotiable: the walk happened even when the day was busy. Especially then.
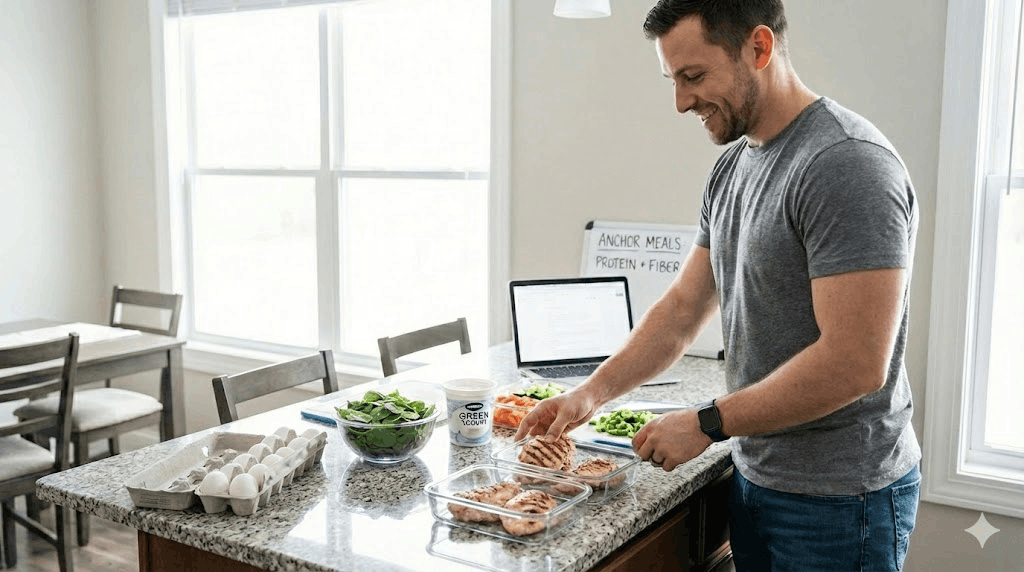
In 2025, the biggest weight-loss regret people report is losing weight and looking worse. The reason is simple: muscle loss. Lena’s plan included strength three days per week.
- Program: full-body sessions built around squats/hinges, pushes, pulls, and carries.
- Progression: adding small amounts of load or reps weekly (not chasing exhaustion).
- Boundary: she stopped doing high-intensity classes during sleep-debt weeks; recovery was treated as a variable, not a moral score.
The ‘GLP‑1 temptation’ moment—and why she waited
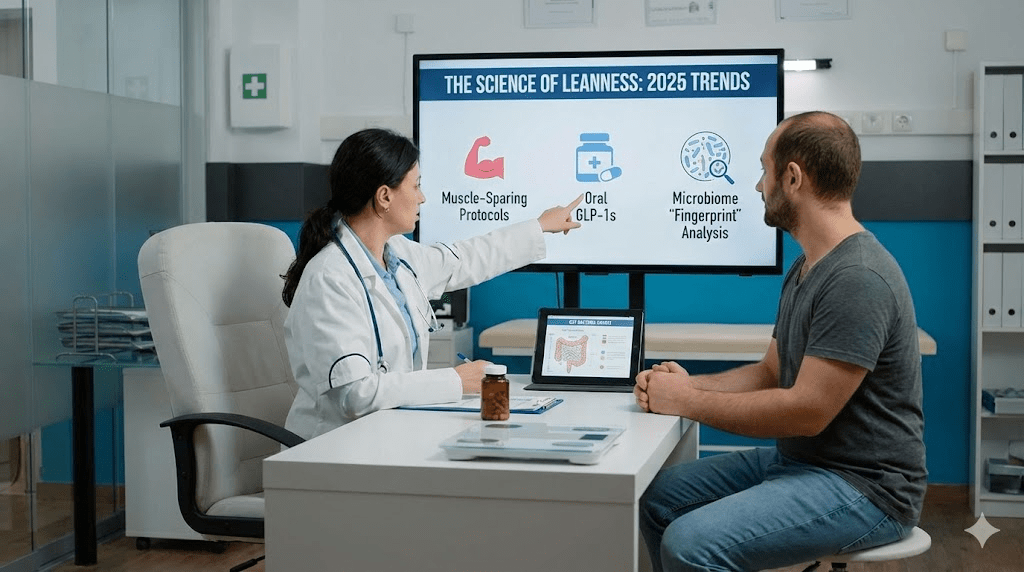
Halfway through, Lena still had cravings some evenings. That’s when the GLP‑1 temptation came back. “I could take a shot and silence this,” she told herself. Her clinician’s response was pragmatic: GLP‑1s can be excellent tools, but they don’t teach the body the skills you need to maintain results.
The plan was: build the habits first, then decide. The logic was muscle-centric: if she ever used an appetite suppressant, she wanted to have strength and protein routines already installed to avoid lean-mass loss.
- If you’re considering GLP‑1s: do it with medical supervision and a muscle-preservation plan.
- If you’re already on GLP‑1s: protein and resistance training are not optional—they are the seatbelt.
Medication can change appetite. It can’t replace strength, sleep, and structure.
What surprised her most
The scale moved, but the better wins were quieter. By week four, her afternoon crash softened. By week six, her cravings were predictable instead of chaotic. By week eight, her waist measurement changed even when the scale plateaued.
- She stopped drinking her carbs. Smoothies became bowls with protein and fiber, or they moved to post‑workout only.
- She built a ‘default dinner.’ A rotating template: protein + veg + one carb portion + a fat. Decisions got smaller, so consistency got bigger.
- She protected sleep like a macro. A caffeine cutoff, a wind‑down alarm, and fewer late workouts.
The plateau (and the adjustment that unlocked it)
At week nine, weight loss stalled. Old Lena would have cut calories harder. New Lena ran a better diagnostic: she looked at steps, sleep, and weekend drift.
- Finding #1: her weekday routine was solid, but weekends had become “social grazing.”
- Finding #2: she was under-recovering after harder strength sessions, which increased appetite the next day.
- Fix: she kept calories roughly stable but tightened structure: a protein breakfast on weekends and a planned treat instead of unplanned nibbling.
Plateaus aren’t proof the plan failed. They’re a signal your system adapted. Adjust the input, don’t panic.
The outcome (and the part most people miss)
Nine months later, Lena was down about 30 pounds. But the more important metric: she could do full pushups again, her waist dropped several inches, and her relationship with food felt… quiet. “It stopped being a daily argument,” she said.
She never became “perfect.” She still ate dessert. She still traveled. The difference was that her baseline was built on muscle, structure, and recovery—not temporary restriction.
A simple template you can borrow
If you want a practical starting point, use this framework for 4–6 weeks and track outcomes (energy, hunger, waist, strength), not just weight.
- Set a protein floor (start with 25–35g per meal, adjust to your body and clinician guidance).
- Walk 10 minutes after two meals daily (or accumulate 20 minutes if life is chaotic).
- Lift 2–3x/week with progressive resistance; keep cardio mostly easy-to-moderate.
- Create a ‘default day’ of meals you can repeat without thinking.
- Protect sleep with one rule (caffeine cutoff, consistent bedtime, or a wind-down alarm).
Common pitfalls
- Chasing calorie perfection before stabilizing protein, steps, and sleep.
- Doing high-intensity workouts on low recovery, then compensating with overeating.
- Using “healthy snacks” as a substitute for meals, creating an all-day insulin drip.
- Assuming a plateau means you should slash food rather than tighten structure and movement.
- Comparing your timeline to someone using medication, genetics, or different stress load.
Practical next steps
- For 7 days, track only three things: protein at each meal, steps, and sleep duration—no calorie counting.
- Choose one lever to tighten first: either a protein-forward breakfast or a daily post-meal walk.
- Add strength training twice per week before adding more cardio volume.
- If you’re considering GLP‑1 medication, discuss a muscle-preservation plan (protein + resistance training) with a qualified clinician.
- If you have symptoms like extreme fatigue, irregular cycles, or rapid unexplained weight gain, consider clinical evaluation for thyroid, iron, glucose regulation, and sleep.
Quick checklist
- I hit a protein source at breakfast and lunch most days.
- I move after meals (even 10 minutes).
- I strength train at least twice weekly.
- My plan includes recovery (sleep is a priority, not an afterthought).
- I judge progress by waist, strength, energy, and appetite—not only scale weight.
Important note: This article is educational and not medical advice. Weight change is influenced by many factors, including medical conditions and medications. If you are pregnant, postpartum, managing an eating disorder history, or have concerning symptoms, work with a qualified healthcare professional.