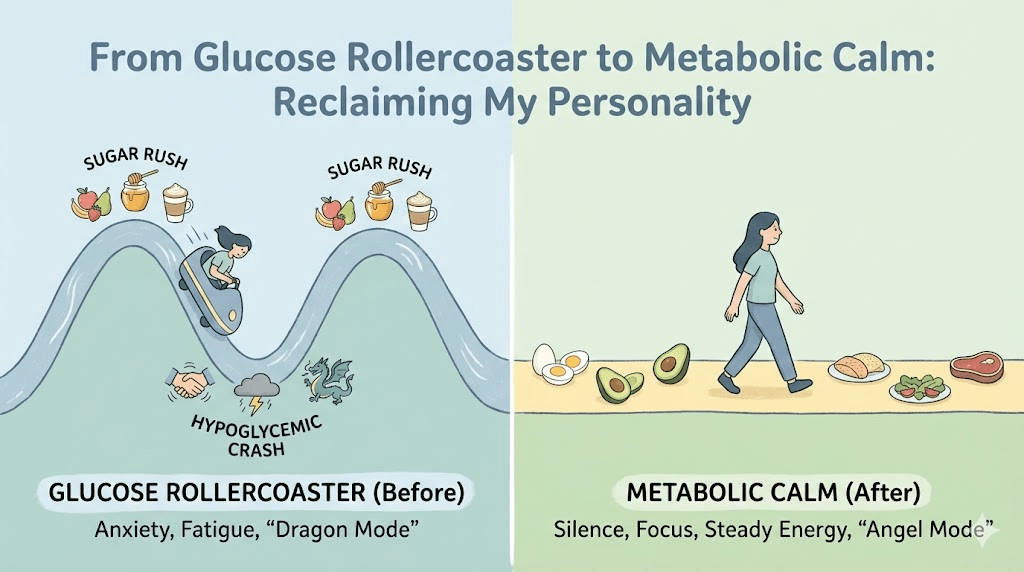
They used to call me the "mood girl". My friends learned the pattern quickly: if I was hungry, they waited. If I had just eaten, I was charming. I thought this was personality. It was physiology.
At 34, I was thin, busy, and quietly exhausted. I blamed my 3:00 PM crash on work. I blamed my 3:00 AM wake-ups on anxiety. I didn’t realize my body was running a daily cycle of spikes, crashes, and rescue hormones—and my brain was paying the price.
My husband joked that I had two operating modes: "Angel" right after eating, and "Dragon" two hours later.
What it looked like from the outside
From the outside, I was functional. I showed up. I delivered. I exercised. But inside, I lived with a background hum of irritability and dread—like I was always one delayed lunch away from becoming a different person.
- Mood swings that arrived on a schedule (often mid-morning and mid-afternoon).
- Brain fog that made simple tasks feel like pushing through mud.
- Cravings that didn’t feel like preferences—they felt like emergencies.
- Nighttime adrenaline: waking up sweaty, heart racing, mind scanning for threats.
The breakfast that started the fire
I did what every well-meaning article told me to do. My mornings started "healthy": oatmeal with honey and fruit, sometimes yogurt, plus a latte. It looked wholesome. It was also a predictable way to launch my blood sugar into orbit.
By 10:30–11:00 AM my hands would tremble. I’d feel suddenly fragile—like the world got louder and harsher. I couldn’t focus. I couldn’t tolerate small inconveniences. My body was asking for fuel with the urgency of a fire alarm.
- I’d grab a cookie or a banana and feel better within 15 minutes.
- Then I’d feel amazing—confident, fast, almost euphoric.
- Then the crash would return, often worse, and the cycle repeated.
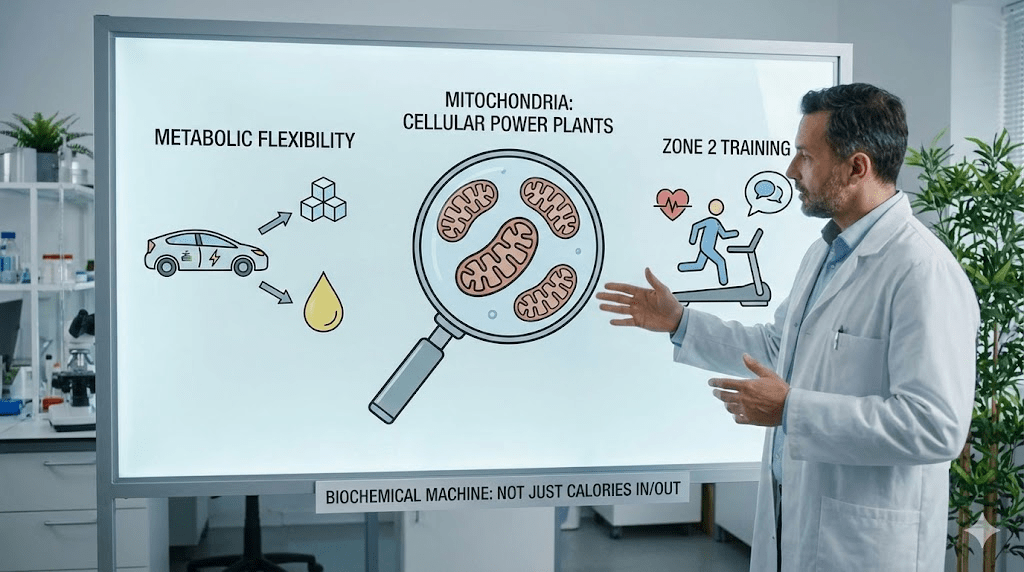
The part I misunderstood
I interpreted the crash as proof I needed more discipline. In reality, it was evidence that my system was overcorrecting. When glucose rises quickly, the body often responds with a big insulin response. For some people, the rebound dip feels like a threat—and the brain reacts accordingly.
When blood sugar drops fast, the body can release adrenaline and cortisol to keep you upright and functioning. That “wired, panicky” feeling is not always psychological. Sometimes it’s your body performing an emergency stabilization.
I didn’t have “random anxiety.” I had predictable physiology—and I was calling it a personality flaw.
The gym blackout
The moment that forced the issue was embarrassing: I fainted mid-workout. Not during a marathon—during a normal training session. The lights went out, I hit the floor, and the trainer handed me a sugary drink like it was a defibrillator.
When I came back, he asked one simple question: “What did you eat before you came?”
"Yogurt and an apple." I said it like it was a virtue.
He nodded and said, "That’s not fuel. That’s a match."
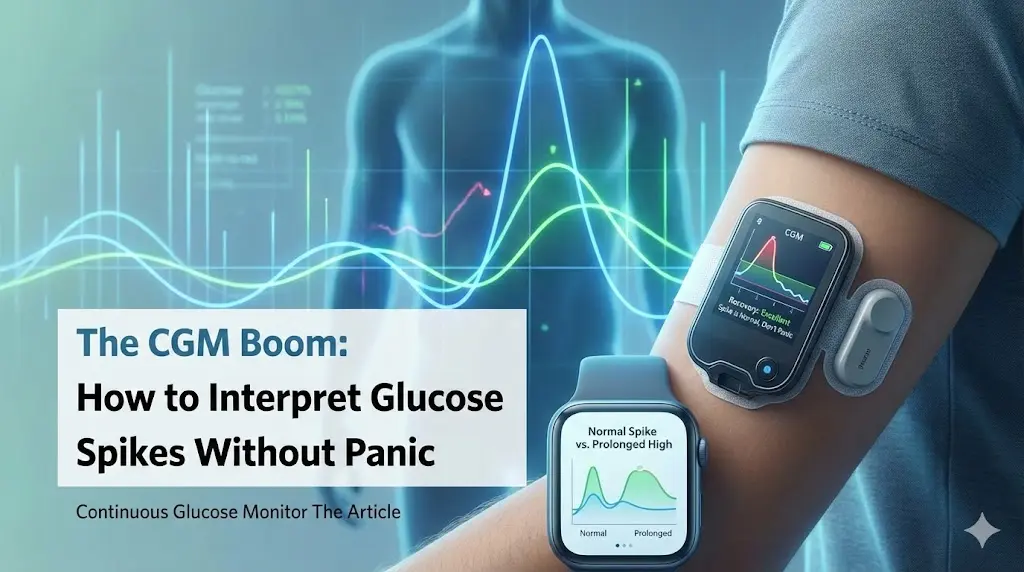
The data that changed my mind
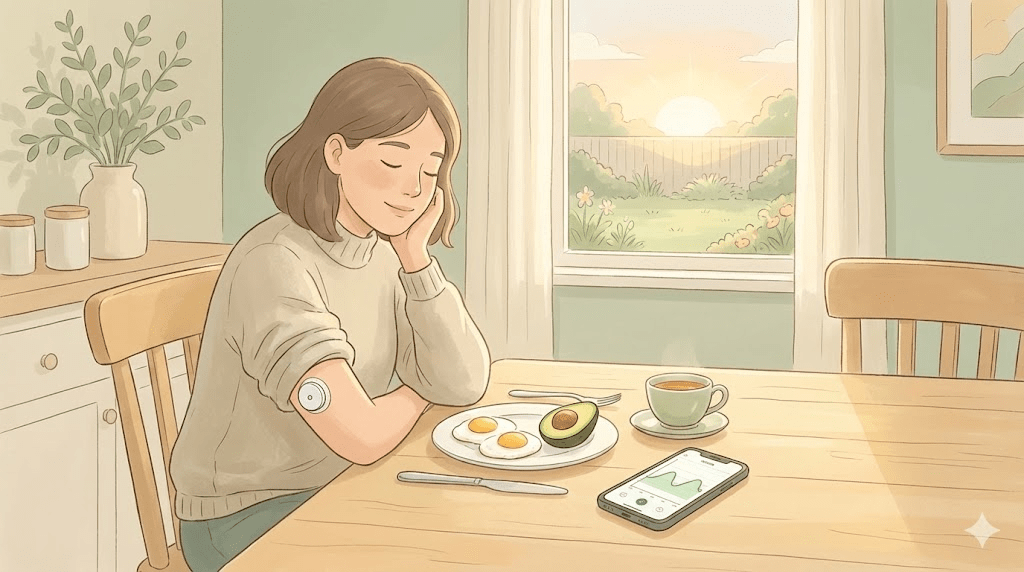
I went to a clinician to rule out obvious issues. But the most useful tool wasn’t a lecture—it was tracking. I wore a glucose sensor for a week (with medical guidance) and finally saw what my body felt every day.
- My “healthy” breakfasts created sharp spikes, then steep drops.
- Coffee on an empty-ish stomach made the swings worse on stressful mornings.
- Hard workouts after sweet breakfasts produced the most dramatic crashes.
The clinician explained it in plain English: my brain was living through repeated mini-emergencies. Each time glucose dipped, my body hit the “panic button” to keep me going. Over time, I started confusing that biochemical surge with who I was.
The 30-day experiment
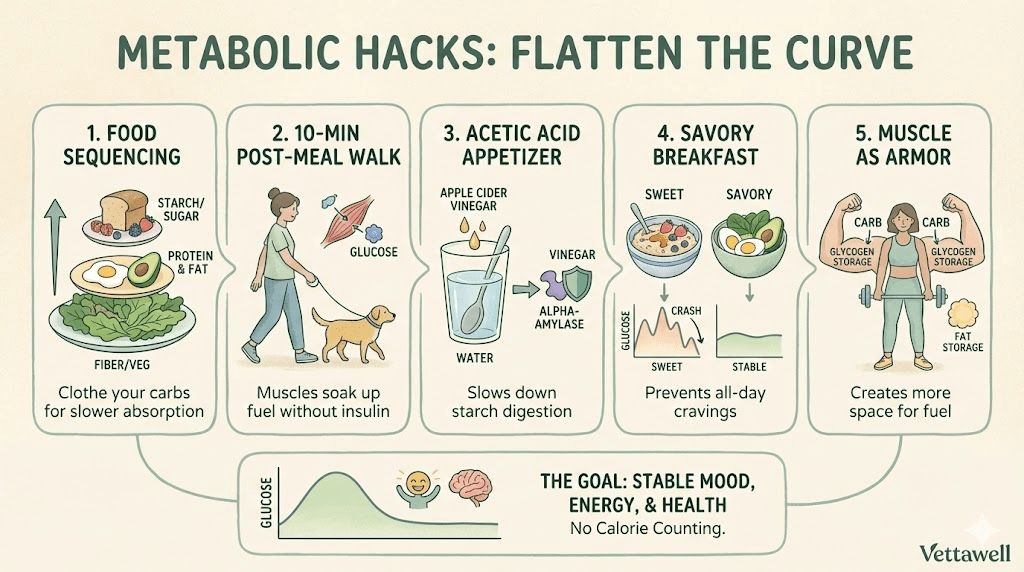
I didn’t “go on a diet.” I ran a controlled experiment: 30 mornings with a different input. No sweet breakfast. No oats, no honey, no pastries, no fruit-first smoothies. I kept it simple: protein, fiber, and fat.
- Eat something savory within 60–90 minutes of waking (no coffee-as-breakfast).
- Build breakfast around protein first (eggs, Greek yogurt plus nuts, tofu scramble, leftover meat/fish).
- Add fiber (berries after protein, chia, flax, vegetables) and healthy fat (olive oil, avocado, nuts).
- If I wanted carbs, I ate them later, paired with protein, and never alone.
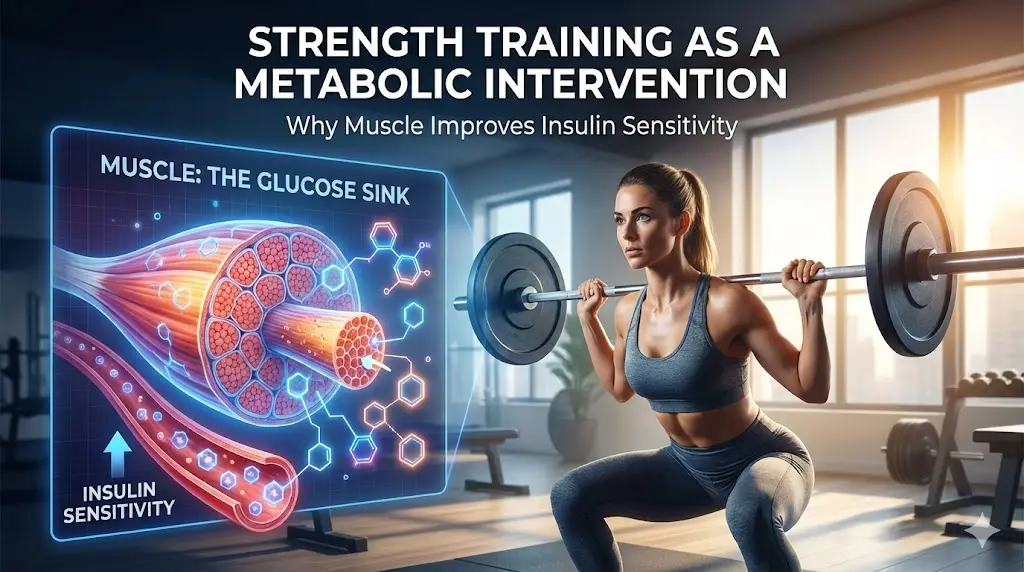
- Walk 8–12 minutes after lunch when possible (movement as glucose management).
The first three days were miserable. My brain had been trained to expect a dopamine-and-glucose surge. Without it, everything felt flat and irritating. I slept poorly. I craved sugar like it was oxygen.
But then something weird happened: the cravings became quieter. The urgency faded. Meals started to feel like nourishment instead of emotional rescue.
The day the noise disappeared
On day five, 3:00 PM arrived and… nothing happened. No fog. No nap fantasy. No desperate hunt for chocolate. I was just… steady.
The best feeling wasn’t energy. It was stability—the absence of the constant internal negotiation with food.
What changed in my body
I didn’t become a different person. I stopped provoking a daily biochemical rollercoaster. When my blood sugar swings smoothed out, my nervous system stopped firing emergency signals all day.
- Mood: fewer spikes of rage and fewer drops into hopelessness.
- Focus: longer stretches of attention without needing a snack to “restart.”
- Sleep: fewer 3:00 AM wake-ups; less sweating and racing thoughts.
- Appetite: hunger felt like information—not like a siren.
My “new” breakfast template
I stopped asking, “What’s the healthiest breakfast?” and started asking, “What keeps my glucose calm?” Here are the breakfasts that worked for me (and for many people who struggle with swings):
- Eggs + avocado + greens (plus berries after).
- Greek yogurt + nuts + chia (sweetness optional, minimal).
- Leftover dinner (yes—salmon and vegetables at 9 AM is allowed).
- Tofu scramble with vegetables and olive oil.
- Protein smoothie that starts with protein + fiber (not fruit-first).
You can still shift the curve without perfection. Start with one move: change the order. Protein and fiber first, sweets last. This alone can reduce spikes for many people.
- Add eggs or yogurt before toast or fruit.
- Pair coffee with food, not an empty stomach.
- Swap granola for nuts/seeds (less sugar, more satiety).
A note on safety
If you have fainting episodes, diabetes, are pregnant, or have an eating disorder history, don’t DIY extreme changes. Work with a qualified clinician. My story is about stability, not restriction.
Practical next steps
- For 7 days, swap to a savory, protein-forward breakfast and note mood/energy at 11 AM and 3 PM.
- Add a 10-minute walk after your largest meal at least 4 days this week.
- Keep “emergency snacks” that stabilize (nuts, cheese, jerky, boiled eggs) instead of sugar-only snacks.
- If symptoms are severe (fainting, palpitations, persistent insomnia), schedule a check-in with a clinician and ask about glucose stability and iron/thyroid markers.
Common pitfalls
- Replacing sugar with “healthy sugar” (smoothies, granola, honey) and expecting different results.
- Going low-calorie and high-intensity—amplifying stress hormones on top of instability.
- Using caffeine as a bandage for a glucose crash, then blaming yourself for the rebound.
Quick checklist
- Breakfast contains protein + fiber most days.
- Afternoon energy is steady (no daily 3 PM collapse).
- Snacking is purposeful, not panic-driven.
- Sleep is improving (fewer adrenaline wake-ups).