At 2:55 PM every weekday, Sarah hit a wall. It wasn’t an abstract “I’m unmotivated” feeling—it was a heavy wave of brain fog and fatigue that made her eyelids feel like lead. She’d stare at her screen and feel her thoughts move through molasses. Meetings became endurance events. By 3:30, she’d be hunting for a fix.
For years, the 42-year-old marketing executive ran the same play: a double-shot latte and a “healthy” granola bar from the breakroom. She would get a short burst of drive, crash again by dinner, and wake up feeling like sleep hadn’t done its job. She wasn’t careless—she was disciplined. Spin class three times a week. Calorie targets that rarely budged. The scale still crept up, and her energy kept shrinking.
“I’m doing everything I’m told to do… so why do I feel worse?”
The pattern behind the crash
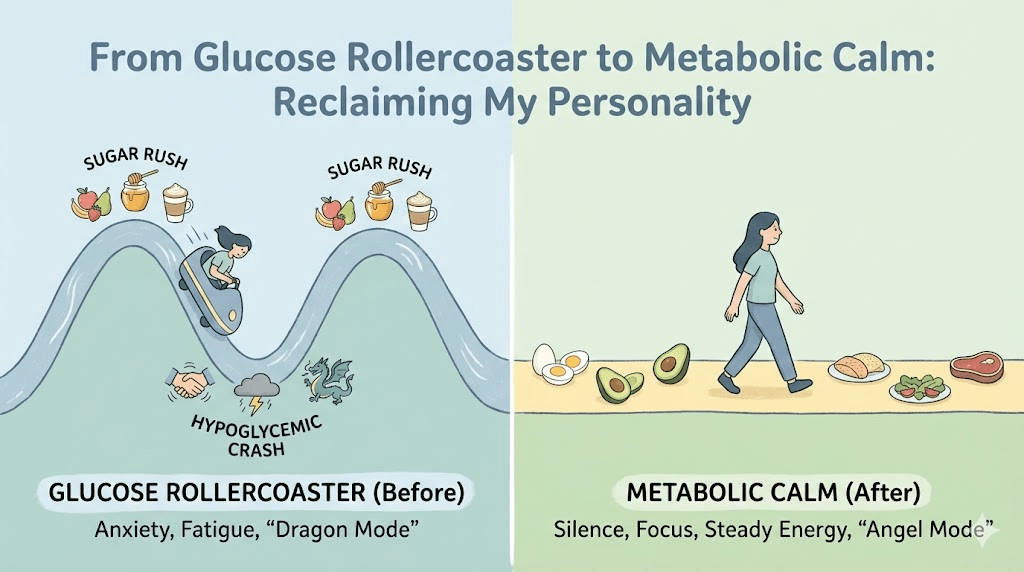
Sarah’s afternoons weren’t random. They followed a predictable loop: a carb-heavy morning, a quick blood-sugar rise, then the inevitable dip—followed by caffeine and more fast carbs to claw back focus. It looked like “productivity hacks.” It was really a fuel problem.
- Morning: “healthy” breakfast that was light on protein and heavy on quick carbs.
- Mid-morning: snack cravings even if she’d eaten recently.
- Afternoon: the crash → caffeine + packaged carbs → temporary lift → bigger dip.
- Evening: depleted willpower, louder cravings, more grazing.
- Next morning: unrefreshed sleep and a repeat of the cycle.
From the outside it can look like overeating or lack of discipline. For Sarah, it felt like her body had stopped cooperating. The phrase she kept using was “inflamed and stuck.”
The wake-up call
The turning point wasn’t dramatic—it was humiliating. In a board meeting, Sarah realized she had read the same slide three times without comprehension. Her brain simply shut off. Not from boredom. From depletion.
Her primary doctor told her it was “part of aging.” Sarah didn’t buy it. She didn’t feel old. She felt dysregulated. So she booked an appointment with a clinician who asked different questions—about her sleep, stress load, cravings, and what her energy looked like across a normal day.
Instead of focusing only on weight and cholesterol, the clinician reviewed metabolic markers (like fasting insulin and triglycerides) and listened to the story her symptoms were telling.
“Sarah, you aren’t overeating. You’re starving on a cellular level—you have fuel, but your body has trouble accessing it.”
Metabolic flexibility, in plain English
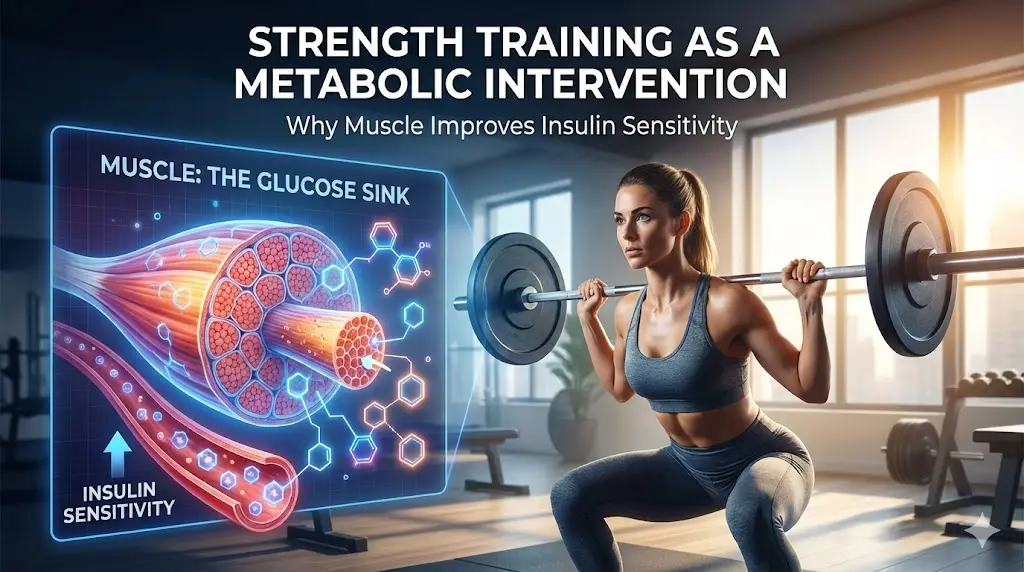
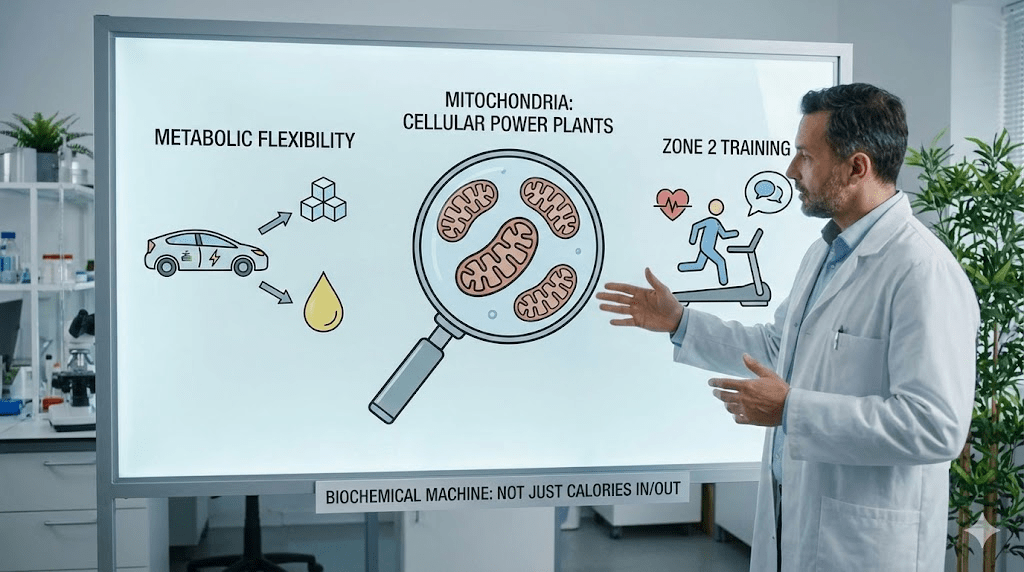
Metabolic flexibility is your body’s ability to switch between fuels—using glucose when it’s available and tapping stored fat between meals or during longer gaps. When you lose that flexibility, your system can become “glucose-dependent.” You feel great right after a carb hit… and terrible when it fades.
This can happen for a lot of reasons: chronic stress, sleep debt, a long history of dieting, highly processed diets, and muscle loss (which reduces your ability to store and use glucose effectively). It’s not about one bad meal; it’s about the operating system running in the background.
The experiment
Sarah’s assignment was terrifying for someone who had counted calories for two decades: stop obsessing over calorie math and start paying attention to stability. The goal wasn’t to eat less. It was to reduce the roller coaster.
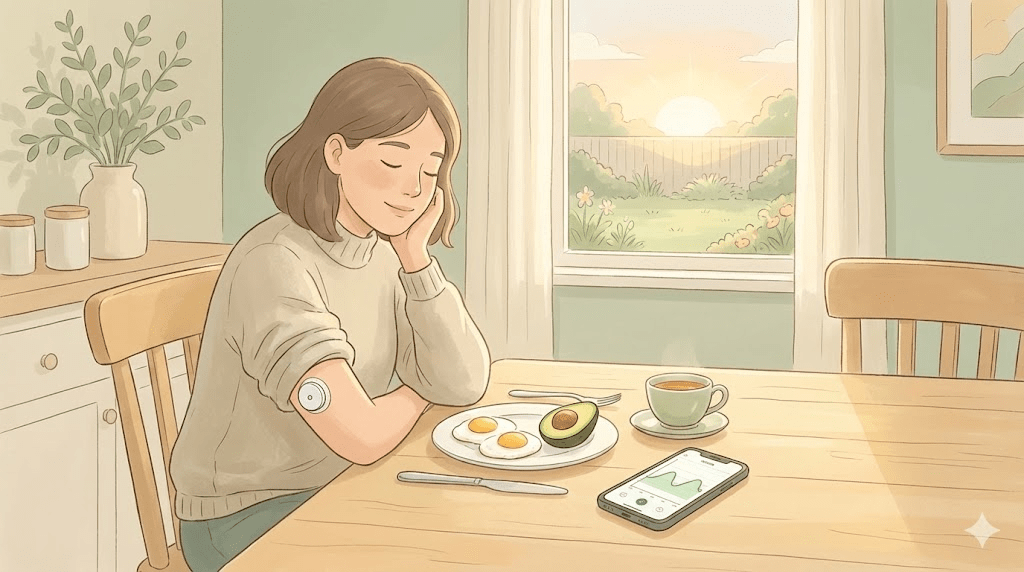
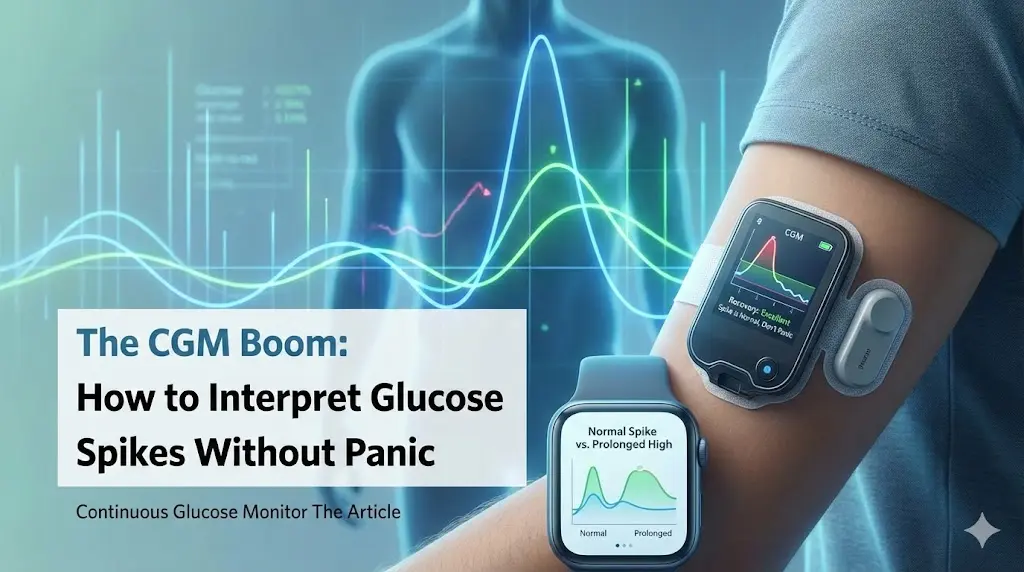
She wore a continuous glucose monitor (CGM) for two weeks to see what was happening under the hood. The results weren’t moral—they were data. And they were eye-opening.
- Her “heart-healthy” oatmeal produced a big spike and a sharp drop that matched her mid-morning hunger.
- The granola bar wasn’t neutral—it lined up almost perfectly with the 3 PM crash she’d fought for years.
- Stress showed up on the graph too: difficult calls and tense meetings changed her numbers even without food.
- When she added protein and fiber, her curve looked smoother—and her cravings got quieter.
“It wasn’t willpower. It was a pattern.”
The shift: an operating system update
Sarah didn’t go on a new “diet.” She made a few strategic switches that changed how her body handled fuel. The first week felt uncomfortable—her body was used to quick hits of sugar. But she treated it like re-training, not punishment.
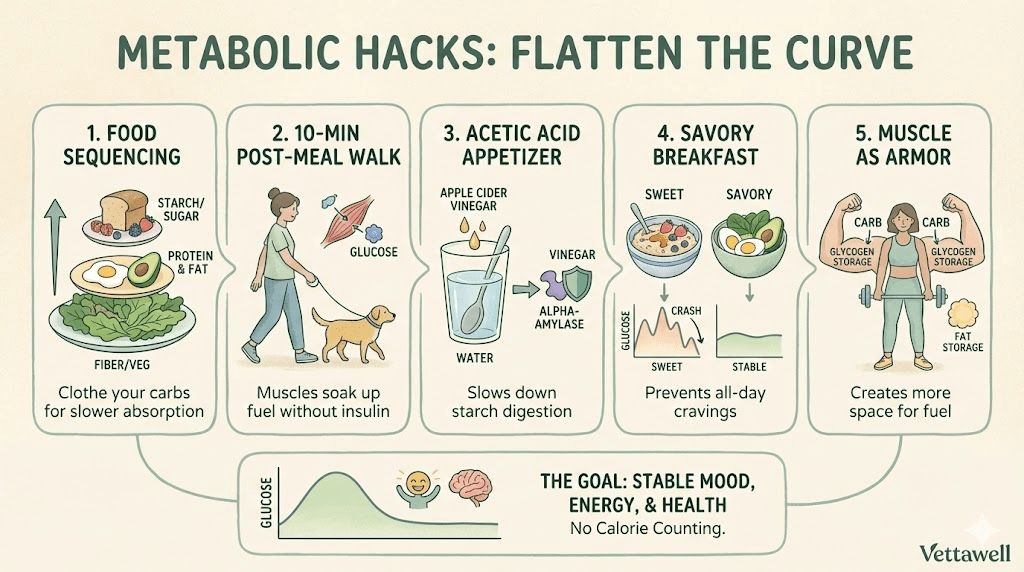
- The savory breakfast: oatmeal became eggs + avocado (or Greek yogurt + nuts + berries). She was surprised to feel steady until lunch.
- The post-meal walk: a 10-minute walk after lunch became her non-negotiable. The CGM showed smaller spikes and fewer crashes.
- Building the engine: she replaced two spin classes with resistance training. Muscle became the “sink” that helped her handle carbs more easily.
She also stopped using caffeine as a rescue. Coffee stayed—but it became a morning tool, not an afternoon emergency. When the crash didn’t arrive, she realized she’d been living in reaction mode for years.
Sarah noticed something else: when she was tense, she craved sugar faster. So she added a two-minute “downshift” after stressful moments—breathing, a short walk, or simply stepping outside. It didn’t eliminate stress, but it reduced the need to self-medicate with food.
The result
The first two weeks were the hardest. Headaches. cravings. irritability. Not because she was “weak,” but because her system was adapting. By week four, something shifted: she woke up one Tuesday and realized she hadn’t hit snooze. The 3 PM wall stopped showing up.
Six months later, Sarah had lost weight—but that wasn’t the headline. Her energy was stable. She could go hours without thinking about food. Her labs improved under clinician supervision. She had enough bandwidth to play with her kids after work. She described it as freedom: trusting her body to fuel her life instead of bargaining with it all day.
Metabolic health isn’t about being skinny. It’s about being steady.
If you see yourself in Sarah, here’s the principle
You don’t need a CGM to learn the core lesson: repeated crashes are often a signal that your system is struggling with fuel switching. The goal is to reduce volatility—especially in the first half of the day—so you’re not “rescuing” your afternoons with caffeine and sugar.
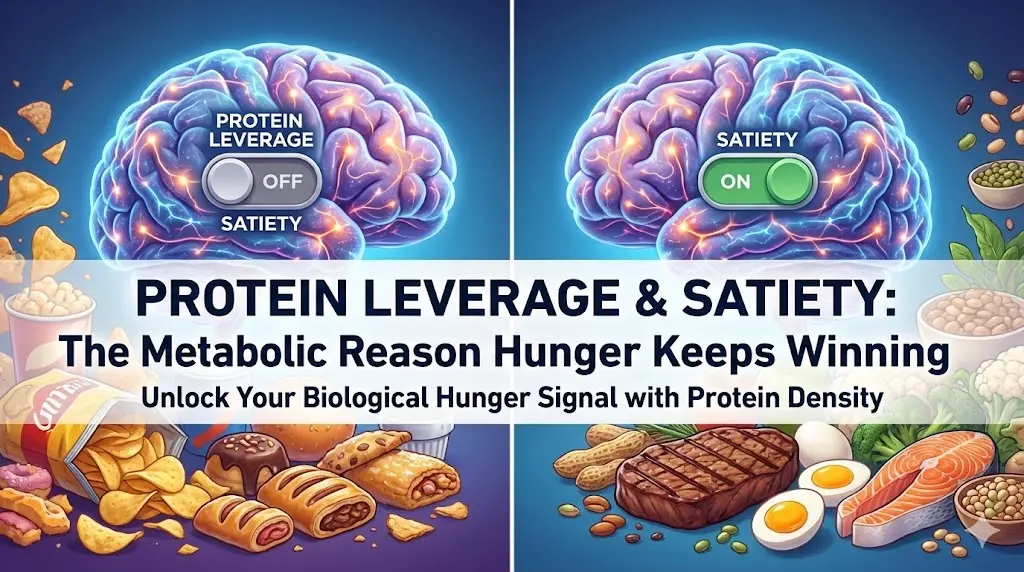
- Anchor meals with protein: it’s the simplest lever for satiety and stability.
- Add fiber and fats for staying power: vegetables, legumes, nuts, olive oil, avocado—whatever fits your diet.
- Move after meals: even 8–12 minutes matters more than intensity.
- Train strength: muscle supports better glucose handling over time.
- Protect sleep: poor sleep makes cravings louder and recovery worse.
A 7-day experiment (simple, not perfect)
Try this as a short experiment to collect data. If you have diabetes, are pregnant, have an eating disorder history, or take medications that affect blood sugar/appetite, work with a qualified clinician before changing your routine.
- Days 1–2: Make breakfast protein-forward (25–35g if feasible) and keep it savory or low-sugar.
- Day 3: Add a 10-minute walk after your largest meal.
- Day 4: Replace one packaged snack with a “stable” option (yogurt, nuts, cheese, fruit + nut butter).
- Day 5: Do one resistance session (or a simple bodyweight circuit) and note your appetite that evening.
- Day 6: Set one sleep lever: earlier bedtime, caffeine cutoff, or phone out of the bedroom.
- Day 7: Review your afternoons: crashes, cravings, mood, focus—what changed?
Common pitfalls
- Using “healthy” sugar (smoothies, granola, fruit-only breakfasts) as a disguised volatility trigger.
- Cutting calories so aggressively that fatigue and rebound hunger become inevitable.
- Skipping resistance training and losing metabolic “storage” capacity over time.
- Treating stress and sleep as optional, then wondering why cravings are unmanageable.
- Fixing breakfast but ignoring lunch structure—leading to an afternoon crash anyway.
Practical next steps
- Start the day with a savory, protein-forward breakfast to reduce glucose volatility.
- Add a 10-minute walk after your largest meal to blunt post-meal spikes.
- Strength train 2–3x/week with a repeatable plan (consistency beats complexity).
- Pick one “crash replacement”: water + protein snack + short walk instead of caffeine + sugar.
- If symptoms are persistent or severe, get medical guidance and consider checking metabolic markers.
Quick checklist
- Breakfast includes protein + fiber (not just carbs).
- Post-meal movement happens often, even if brief.
- Snacking is reduced or purposeful—not a panic response.
- Strength training is in the plan, not “when I have time.”
- Energy is steadier across the day (fewer rescue tactics).