“It’s okay not to be okay.” In 2025 the question is: what’s the fastest, most repeatable way to get back to “okay” when the system is overloaded?
For the last decade, the mental health conversation was about destigmatization. “It’s okay not to be okay.” In 2025, the conversation has shifted to implementation. We know we aren’t okay. The question is what we can do today—without a six‑month waitlist, without perfect circumstances, and without pretending that stress is only a “mindset” problem.
This guide breaks down The 2025 Mental Health Report: AI Therapists, Psychobiotics, and the End of "Talking It Out" into the mechanisms and decision points that matter in real life. The big theme of this year is simple: mental health is no longer treated as a single lever (talking). It’s treated as a system—biology, behavior, and belonging.
Key takeaways
- 2025 is the year of systems, not slogans: sleep, food, movement, connection, and tools that scale.
- The fastest wins come from treating anxiety/depression as physiology (inflammation, circadian rhythm, blood sugar, nervous system tone).
- AI is becoming the first responder for journaling, CBT prompting, and panic de-escalation—useful, but not a replacement for clinicians.
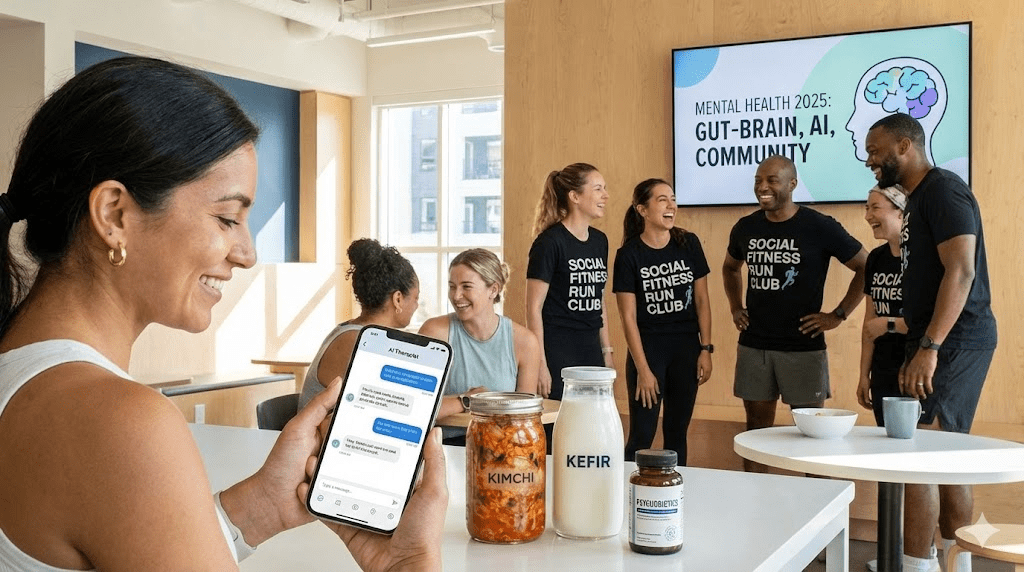
- “Psychobiotics” and nutritional psychiatry are moving from niche to mainstream: mood care is increasingly a gut-brain protocol.
- Loneliness is now treated like a health risk factor: 2025’s solution is structured socializing, not “more me-time.”
Why 2025 feels different
Two realities collided: demand exploded, and supply stayed flat. More people are seeking help, while therapist availability has not scaled at the same rate. The result is a new hierarchy of care: fast-access tools first (AI + self-guided), then targeted human care (group therapy, coaches, clinicians) once you can get in.
This shift is not purely technological. It is philosophical. The old model assumed that insight alone could fix distress. The 2025 model assumes many symptoms are outputs of disrupted inputs—sleep debt, isolation, metabolic instability, inflammatory diets, and constant digital stimulation.
Trend 1: The Rise of “Psychobiotics” and Nutritional Psychiatry
We have known about the gut‑brain axis for years. What changed is the way clinicians talk about it: not as a fun fact, but as a treatment pathway. Your gut lining, immune system, and microbial ecosystem are now viewed as upstream levers for mood, focus, and stress tolerance.
- The clinical reality: A meaningful portion of patients do not achieve adequate relief from first‑line antidepressants, driving demand for adjunctive strategies.
- The mechanism: The gut influences the brain through inflammation, vagus‑nerve signaling, microbial metabolites (like short‑chain fatty acids), and neurotransmitter precursors.
- The emerging tool: “Psychobiotics”—specific probiotic strains and prebiotic fibers aimed at stress regulation and mood support—are being studied as add‑ons, not magic replacements.
What this looks like in practice
The new baseline protocol in many 2025 playbooks is boring, but effective: stabilize blood sugar, repair the gut barrier, reduce ultra‑processed foods, and increase fiber diversity. The headline is not “take a pill.” It’s “change the environment that your nervous system lives in.”
- The food upgrade: fermented foods (kefir, yogurt, kimchi, sauerkraut) plus fiber sources (beans, oats, berries, flax/chia) scaled slowly to tolerance.
- The inflammation filter: reduce alcohol, liquid sugar, and frequent late‑night snacking—three major drivers of sleep fragmentation and next‑day anxiety.
- The supplement reality check: strains and responses vary; this is not a one‑size‑fits‑all aisle at the pharmacy.
Trend 2: AI as the “First Responder” for Mental Triage
AI is not replacing therapists. It is replacing dead air—those months where a person is suffering with no support between now and the first appointment. In 2025, the most common use case is practical: guided journaling, CBT reframes, values clarification, exposure planning, and panic de‑escalation in the moment.
- Why it works for many people: availability, zero friction, and repetition. The nervous system changes through reps, not inspiration.
- What it’s best for: mild to moderate anxiety, habit tracking, thought labeling, and building a daily “mental hygiene” routine.
- Where it’s risky: crises, complex trauma, psychosis/mania, eating disorders, and situations requiring mandatory reporting or clinical judgment.
The 2025 AI rulebook
- Use it like a coach, not a judge: prompt it to ask questions, not to deliver verdicts.
- Pick tools with privacy defaults: prefer products that clearly state retention rules and data handling. Assume anything you type could be stored unless told otherwise.
- Anchor to a protocol: CBT worksheets, exposure ladders, and behavioral activation plans outperform vague “venting.”
- Escalate fast: if symptoms worsen, functioning drops, or safety concerns appear, move from tool to clinician.
The deeper shift here is cultural: therapy is no longer treated as a weekly conversation. It is treated as a daily practice, and AI provides the scaffolding for that practice when humans aren’t available.
Trend 3: The End of “Talking It Out” as the Primary Strategy
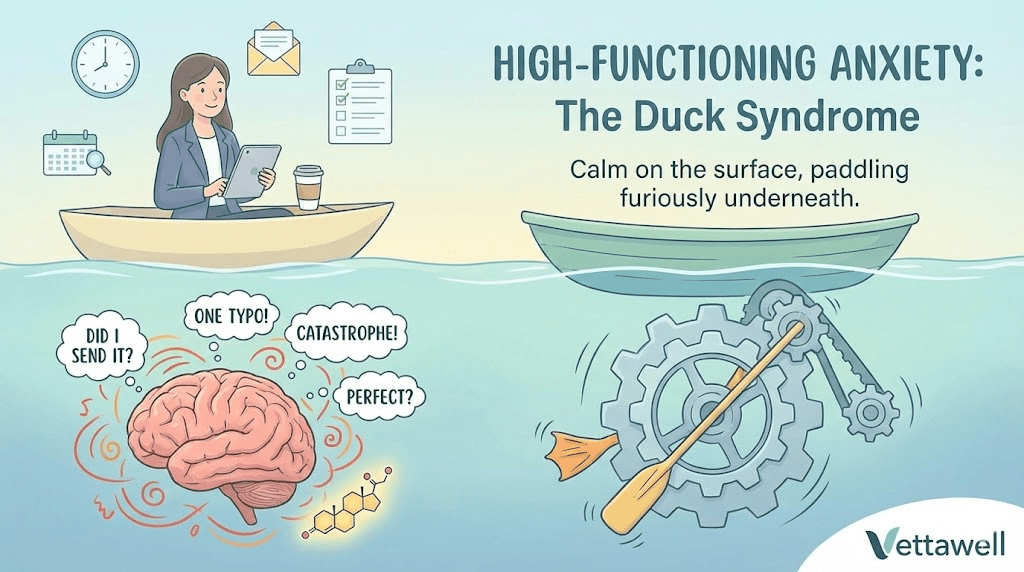
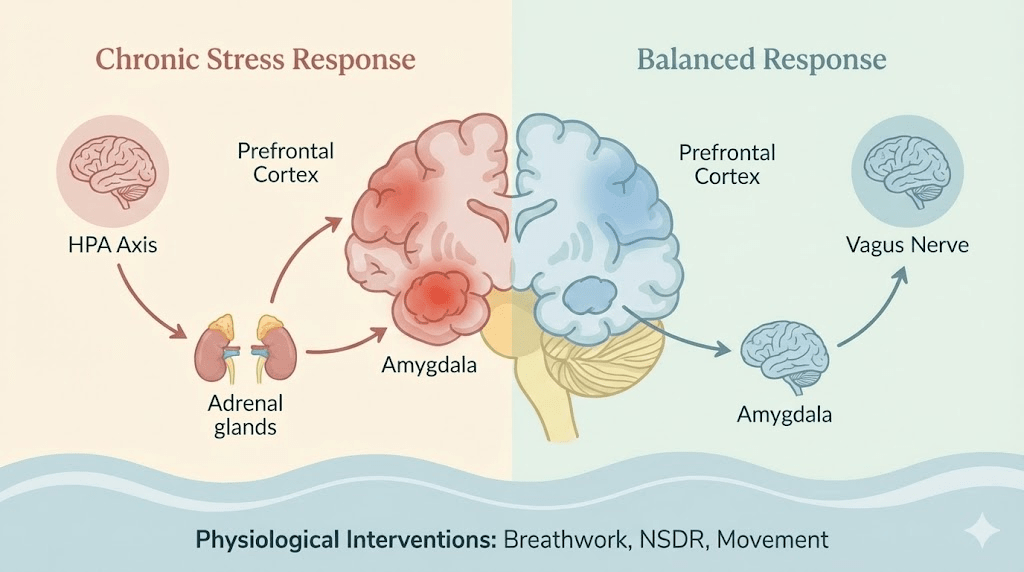
2025 doesn’t reject talk therapy. It rejects the idea that talk therapy is sufficient on its own. The body keeps score, and many modern symptoms are body‑driven: dysregulated sleep, chronic cortisol elevation, glucose volatility, and reduced vagal tone from isolation and screen exposure.
- The reframe: anxiety is often an arousal problem; depression is often an energy and meaning problem; both are often sleep problems.
- The upgrade: integrate somatic interventions (breathwork, movement, cold/warm contrast, progressive muscle relaxation) with cognitive tools.
- The outcome target: fewer symptoms, faster recovery from stressors, and higher baseline resilience—not perfect happiness.
Trend 4: “Social Fitness” and the Loneliness Countermeasure
Loneliness has moved from “sad” to “clinical.” Remote work, mobility, and digital substitution weakened the everyday contact that used to regulate our nervous systems. 2025’s response is not to wait for friendship to happen. It is to build it like a training plan.
- Structured socializing: run clubs, co‑working cafés, “reading parties,” and recurring small rituals that remove decision fatigue.
- The low‑pressure format: short calls and lightweight check‑ins that don’t require a two‑hour life update.
- Co‑regulation: shared meals, walks, and group movement outperform isolated “self‑care” when stress is the issue.
If the last decade sold self‑care as a product, 2025 treats social connection as a behavioral vitamin. Not optional. Not indulgent. Preventive.
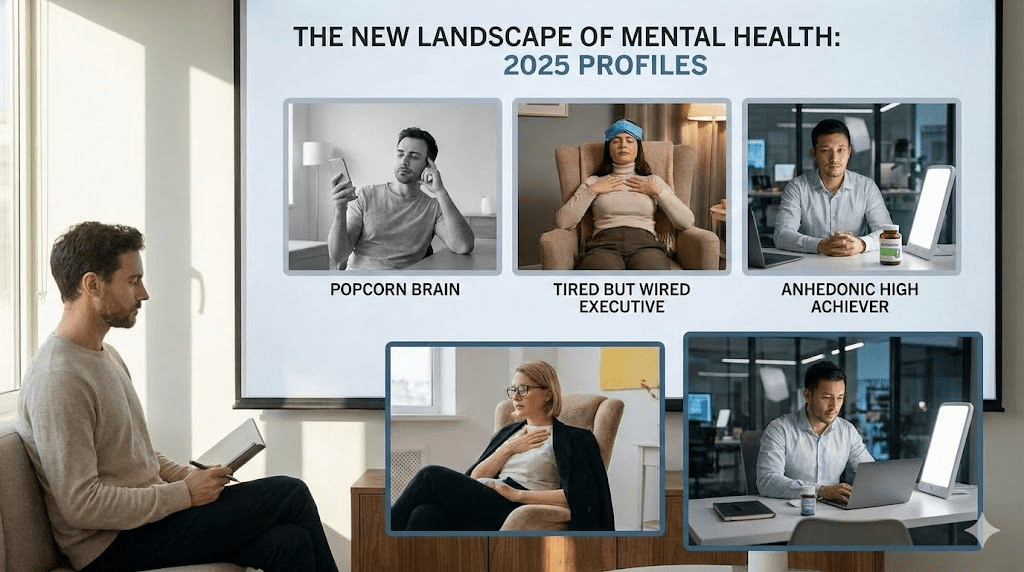
The missing conversation: attention, dopamine, and burnout
A major driver behind rising anxiety is not just “stress.” It’s attention fragmentation. Constant context switching trains the brain to live in a partial‑focus state, which feels like unease. The mind interprets fragmented attention as unsafety.
- The symptom cluster: irritability, low patience, brain fog, and the feeling of being “behind” even when you’re working nonstop.
- The intervention: a daily block of single‑task focus plus an evening “dopamine taper” (less novelty, fewer screens, lower stimulation).
- The result: better sleep onset, reduced rumination, and improved emotional regulation the next day.
A practical 2025 framework: the 3-Layer Reset
Most people try to fix mental health at the top layer (thoughts). The 2025 playbook starts lower—inputs first—then moves up. Use this three‑layer framework to diagnose what you actually need.
- Layer 1 — Biology: sleep consistency, nutrition, alcohol, movement, sunlight, and basic medical causes (thyroid, iron, B12, apnea).
- Layer 2 — Nervous system: downshift tools (physiological sigh, long exhale breathing, paced walking, muscle release) and stimulation hygiene.
- Layer 3 — Meaning & belonging: relationships, boundaries, purpose, and work design.
Practical next steps
- Pick one scalable tool for daily practice (AI journaling prompts or a CBT worksheet) and use it for 10 minutes a day for 14 days.
- Run a “gut + mood” experiment: add one fermented food and one fiber source daily for 2 weeks, tracking sleep and irritability.
- Create a social ritual you can repeat weekly (walk + coffee, class, club). Treat it like training, not a vibe.
- Protect a consistent wake time for the next 14 days (weekends included).
Common pitfalls
- Trying to “think” your way out while sleep and blood sugar remain unstable.
- Using AI as a substitute for crisis support or complex clinical care.
- Adding 10 new interventions at once and quitting all of them by day 4.
- Confusing isolation with recovery: rest is not the same as disconnection.
Quick checklist
- Wake time is stable (±30 minutes).
- Daily movement happens (a walk counts).
- One downshift tool is practiced (long exhale breathing, NSDR, or a short body scan).
- One social touchpoint is scheduled each week.
- Stimulation is reduced at night (less scrolling, fewer late‑night work pings).