This guide breaks down The 2025 Clinic Report: 3 New Mental Health Crises (and the Protocols We Use to Fix Them) into the mechanisms and decisions that matter in practice. The mental-health landscape has shifted dramatically—not just in diagnoses, but in what actually works inside the constraints of real life (time, attention, screens, stress).
In 2025 we stopped asking only, “What are you thinking?” and started asking, “What is your system doing?”
Key takeaways
- Most 2025 cases are not “mystery personalities.” They’re predictable neurobiological adaptations to overload (dopamine, sleep, inflammation, social isolation).
- We triage by state first (arousal, shutdown, sleep) and story second (thoughts, narratives).
- Protocols that work best combine a digital boundary, a somatic downshift, and a physiology lever (light, movement, food, breathing).
- The 2025 takeaway: mental health is increasingly treated as physical systems engineering, not willpower.
What changed in 2025
A decade ago, the “big two” in outpatient clinics were generalized anxiety and major depression. In 2025, we still treat those—yet the dominant presentations often look different: attention fragmentation, sleep-wired exhaustion, and emotional flatness that resembles depression but behaves like inflammation or dopamine depletion.
- A new umbrella concept: Acquired Neuro-Divergence — brains re-shaped by chronic digital stimulation, disrupted circadian cues, and persistent stress physiology.
- Why it matters: many patients blame character (“I’m lazy,” “I’m broken”), while the drivers are environmental and reversible with the right levers.
How we triage in the clinic
Before prescribing anything, we run a simple triage. It prevents months of mismatched treatment (for example, trying CBT when a patient is physiologically frozen, or chasing a supplement stack when the real issue is sleep apnea or late-night light).
- Step 1 — Arousal state: Are you in fight/flight (wired), freeze (stuck), or shutdown (numb)?
- Step 2 — Sleep integrity: Duration, timing, awakenings, snoring/apnea risk, and whether mornings feel restorative.
- Step 3 — Dopamine load: How many micro-hits per hour (notifications, short video, multitasking)?
- Step 4 — Inflammation signals: GI symptoms, chronic pain, ultra-processed diet, low sunlight, sedentary baseline.
- Step 5 — Safety screen: suicidality, self-harm, mania, psychosis, substance dependence. If present, the protocol changes immediately.
Crisis 1: The “Popcorn Brain”
Case profile: Mark, 32 (Creative Director). He reports, “I think I have early-onset dementia. I can’t watch a movie without grabbing my phone. I can’t read two pages. My mind jumps like popcorn.”
In our clinic, this often maps to Acquired Attention Deficit (AAD)—not genetic ADHD, but attention systems conditioned by high-frequency novelty (short video, constant tabs, rapid task switching). The brain becomes allergic to low-stimulus tasks because the reward threshold has been pushed upward.
What’s happening biologically
- Dopamine threshold drift: novelty becomes the only reliable “on switch.”
- Attention switching tax: frequent context-switching increases perceived effort and decreases task persistence.
- Sleep + screens feedback loop: late-night stimulation reduces deep sleep; reduced sleep worsens impulse control and attention.
Protocol: Dopamine Resensitization (the “Boring Hour”)
Standard meditation can fail at first because the noise is not “thoughts”; it’s a nervous system trained for stimulus. So we prescribe a graded reset: lowering the stimulation floor until ordinary life becomes rewarding again.
- Grayscale + notification triage: remove color cues; keep only human-critical notifications.
- The “Boring Hour” (daily): one hour with no phone, no podcasts, no music, no multitasking. Walking, tidying, staring out a window all count.
- Single-task block (20–40 min): one tab, one task; timer visible; break without the phone.
- Replacement pleasure: choose one low-dopamine hobby (paper book, sketching, cooking) and make it the default “break.”
Clinical note: the goal is not to become anti-technology; it is to restore voluntary attention. Patients often report that reading becomes “possible” again within a few weeks, not because their personality changed, but because their baseline stimulation requirement dropped.
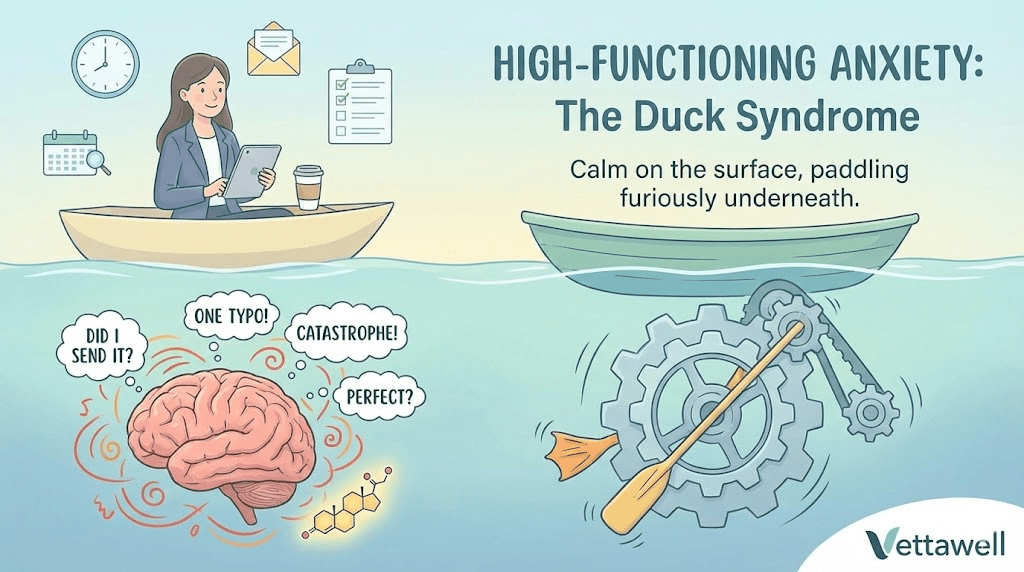
Crisis 2: The “Tired But Wired” Executive
Case profile: Elena, 44 (VP of Operations). “I’m exhausted all day, but at night my heart races. I grind my teeth. I’m tight even after massages.”
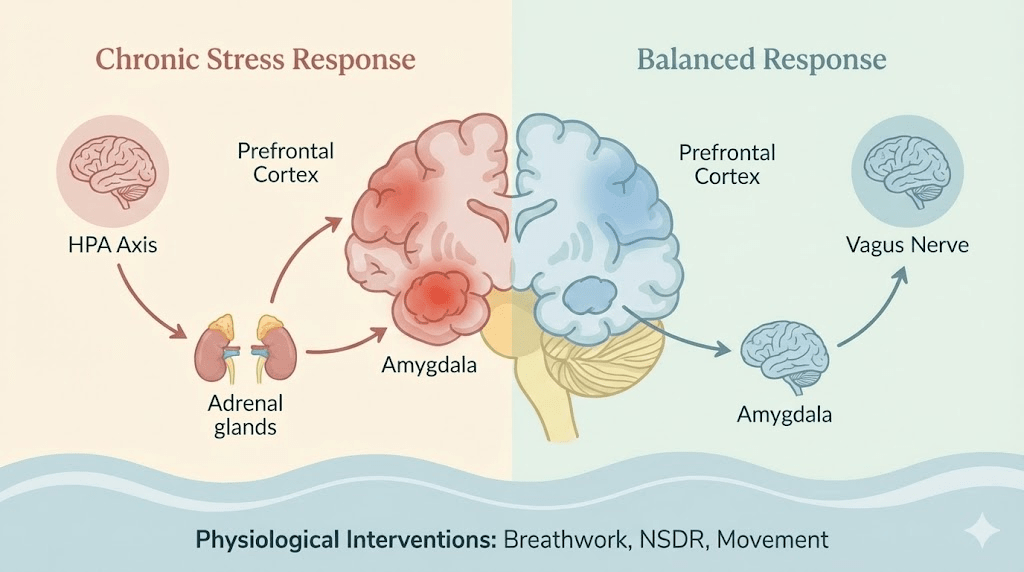
This is frequently Sympathetic Dominance with a functional freeze overlay: the system is simultaneously pushing gas (anxiety) and brakes (shutdown). Talk therapy alone may not move the needle because the bottleneck is autonomic physiology.
What we see in real life
- Sleep initiation issues: mental fatigue with physical hyperarousal (jaw, chest, gut).
- Rest that doesn’t restore: weekends don’t reset the system.
- Stress that isn’t “mental”: even neutral events feel like threats because the baseline is already elevated.
Protocol: Somatic “Bottom-Up” downshifts
We stopped trying to “think” our way out of stress. We teach the body a faster language: breath, temperature, posture, and rhythm. These tools are designed to be deployable during real workdays, not only during a perfect wellness routine.
- Physiological sighs (2–5 minutes): double inhale through the nose + long exhale, repeated. Useful before meetings or difficult conversations.
- Cold face/chest exposure (20–60 seconds): brief cool water or cold pack to trigger a rapid downshift (not a toughness contest).
- Orientation drill (60 seconds): slowly scan the room, name objects, and feel feet on the floor—signals “no immediate danger” to the brainstem.
- TRE-style tremoring (2–10 minutes): guided lower-body shaking to discharge stored arousal (best taught by a trained provider).
- Boundary medicine: a hard stop time for work messages; without it, no technique can compete.
Implementation detail: we prescribe “minimum viable downshift.” One tool, done consistently, beats a perfect routine done twice. For high performers, compliance improves when the tool is framed as performance engineering rather than self-care.
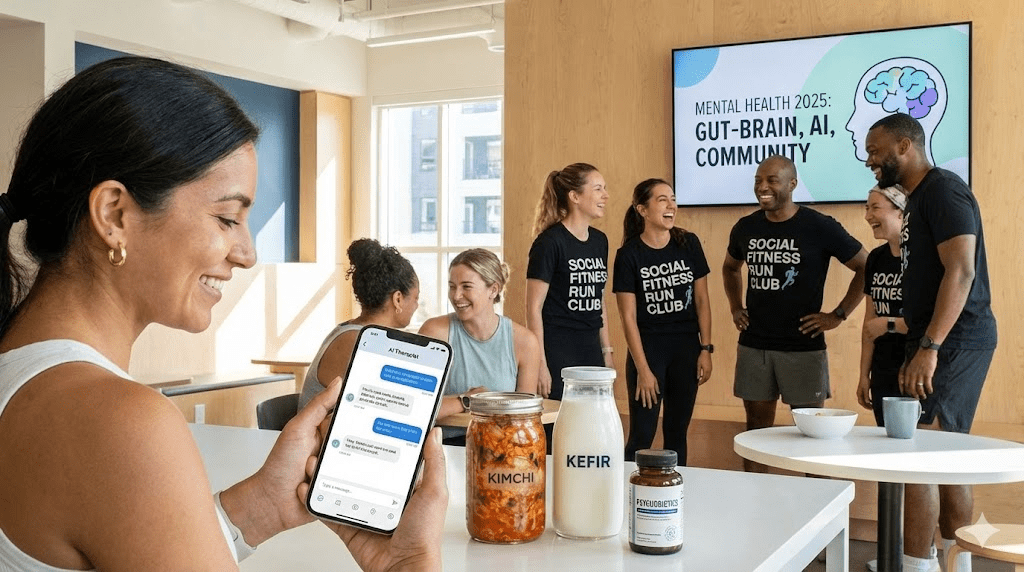
Crisis 3: The “Anhedonic” High Achiever
Case profile: David, 28 (Software Engineer). “I’m successful, I have friends, but I feel nothing. It’s like the volume of life is stuck at 10%.”
This presentation often looks like depression, but behaves like neuro-inflammation or metabolic depletion: sleep is irregular, sunlight exposure is low, food is ultra-processed, and movement is minimal. The brain shifts into a conservation mode—a pattern sometimes described as “sickness behavior.”
Clues that this is inflammation-driven, not purely cognitive
- Body signals: GI symptoms, frequent infections, skin flares, persistent aches.
- Circadian mismatch: late light, late wake, and weak morning cues.
- Food pattern: high refined carbs + low fiber/protein; irregular meals; reliance on stimulants.
- Mood pattern: emotional flatness more than sadness; enjoyment returns briefly after movement or time outdoors.
Protocol: Psychonutrition + circadian repair
We treat the gut-brain axis and the circadian system in parallel. The objective is not “happy thoughts”; it’s lowering inflammatory load, restoring neurotransmitter precursors, and re-establishing day-night signaling.
- Fermented-food anchor (daily): kefir, yogurt, kimchi, sauerkraut—start small if sensitive.
- Fiber target (most days): legumes, vegetables, oats, chia; increase gradually to avoid GI backlash.
- Omega-3 emphasis: fatty fish or clinically appropriate supplementation when diet is insufficient.
- Morning light (10–20 minutes): outdoor light soon after waking; even cloudy days matter.
- Post-meal movement (10 minutes): walk after the largest meal to improve glucose handling and energy stability.
- Caffeine boundary: no later than early afternoon for most patients; sleep quality is the keystone.
Clinical note: if anhedonia is severe, persistent, or accompanied by suicidal thoughts, this protocol is supportive—not a substitute for professional psychiatric assessment. We treat physiology while ensuring safety and appropriate escalation.
What we do differently than 2020-era mental health
- We measure and track: sleep timing, screen minutes after 9 PM, step count, and morning light exposure—simple inputs with outsized impact.
- We design environments: fewer notifications, fewer default dopamine spikes, fewer late-night cues. The goal is not discipline; it’s friction.
- We prioritize “state regulation” over insight first: insight becomes useful once the system is stable.
Red flags that change the plan immediately
- Suicidal thoughts, self-harm, or intent to harm others.
- Manic symptoms (reduced need for sleep, grandiosity, risky behavior) or psychosis.
- Severe substance dependence or withdrawal risk.
- Snoring with daytime sleepiness, witnessed apneas, or high blood pressure (possible sleep apnea).
- Rapid unintended weight loss, persistent fever, or neurological deficits.
If any red flags are present, we escalate to appropriate medical care rather than “self-optimizing.” Protocols are tools, not replacements for diagnosis and safety.
The 2025 takeaway
The biggest shift this year is acknowledging that mental health is physical health. The brain is not floating in a jar. Attention, mood, and resilience are outputs of sleep architecture, nervous system tone, inflammatory load, and the dopamine environment. When we treat those inputs, many “mysterious” symptoms become predictable—and treatable.
Practical next steps
- Pick one lever for 14 days: (1) morning light, (2) the boring hour, or (3) a daily physiological sigh routine.
- Set one digital boundary that is non-negotiable (e.g., no short-form video after 9 PM).
- Add one recovery behavior that happens even on busy days (10-minute walk, 5-minute breath, or a hard shutdown ritual).
Common pitfalls
- Trying to out-think dysregulation while sleep, light, and stimulation remain unchanged.
- Doing ten interventions for three days, then quitting—rather than one intervention for three weeks.
- Using stimulants to push through shutdown and then treating the crash as a character flaw.
Quick checklist
- Sleep is protected most nights (duration and timing).
- Daily movement happens (a walk counts).
- One nervous-system downshift tool is practiced.
- Work and phone boundaries are explicit and consistent.
- If symptoms are severe or worsening, a qualified clinician is involved.