Urinary leakage has become a punchline: the mom who can’t jump on a trampoline, the runner who crosses her legs when she sneezes, the friend who “knows every bathroom” in town. But normalizing symptoms doesn’t make them inevitable. Pelvic floor physical therapists repeat a simple truth: common does not mean normal—and the default advice to “do more Kegels” is often the wrong first move.
Common does not mean normal.
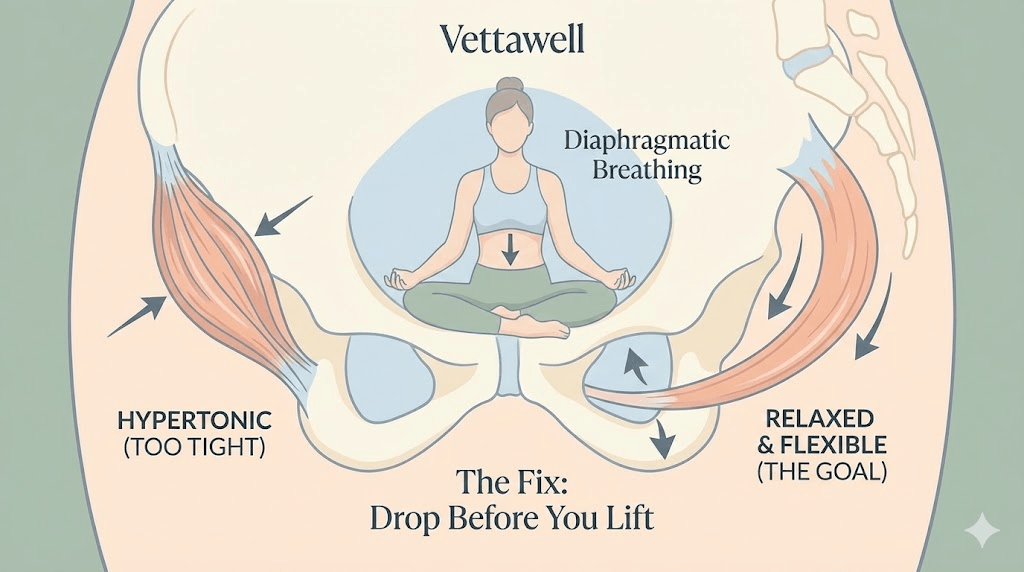
Kegels are not inherently bad. The problem is the one-size-fits-all assumption that every pelvic floor issue is caused by weakness. In reality, pelvic floor dysfunction often comes from poor coordination, excessive tension, or a lack of range of motion—not just a lack of strength. If a muscle is already clenched and fatigued, asking it to squeeze harder can worsen symptoms.
Key takeaways
- The pelvic floor is not a static “shelf.” It’s a dynamic system that needs strength + flexibility + timing.
- Some symptoms improve with strengthening; others improve by learning to relax and lengthen first.
- A hypertonic (too-tight) pelvic floor can cause leakage, urgency, constipation, and pain—yes, even when it’s “strong.”
- Breathing and nervous system state matter: chronic stress can translate into chronic pelvic tension.
- The fastest path is assessment: a pelvic floor PT can identify whether you need down-training, strengthening, or coordination work.
The "hammock" myth (and what the pelvic floor really does)
Many people picture the pelvic floor as a simple hammock holding organs in place. A better model is a trampoline: it must support downward pressure, absorb impact, and then rebound. It works as part of a team with the diaphragm, deep abdominals, hips, and spine.
On a normal inhale, the diaphragm descends. Ideally, the pelvic floor gently yields and lengthens. On the exhale, the system recoils and supports. Strength helps—but only when the muscle can also relax, move, and respond quickly.
Think of holding your bicep flexed all day while carrying a grocery bag. The muscle becomes shortened, tired, and reactive. If someone told you to fix elbow pain by flexing harder, it would sound ridiculous. Yet many women are told to fix pelvic symptoms by squeezing a muscle that may already be gripping all day.
Two different problems that look similar
Pelvic floor issues can share symptoms, but the underlying pattern can be very different. A simplified framework:
- Often associated with: postpartum recovery, connective tissue laxity, certain surgeries, or deconditioning.
- Common experience: less support against pressure (jumping, coughing, lifting).
- Typical needs: strength + coordination, not endless reps.
A hypertonic pelvic floor is shortened and tense—sometimes due to chronic stress, heavy training, habitual gripping, pain avoidance, or compensation for weak core/hip mechanics. Tight tissue can still be weak in function because it can’t contract and relax efficiently.
- Common experience: urgency, frequency, pain, constipation, “can’t fully empty,” or leakage that makes no sense.
- Why leakage can happen: a rigid muscle doesn’t react well to sudden pressure; it can’t “snap” closed when you sneeze or land.
- Typical needs: down-training (relaxation + range of motion) before strengthening.
A muscle that can’t relax is a muscle that can’t truly get stronger.
Signs your pelvic floor might be too tight (not too weak)
- Pain with intercourse, penetration, or tampon insertion.
- Frequent urge to urinate even when the bladder isn’t full.
- Constipation or straining, or a sense of incomplete emptying.
- Lower back, hip, or tailbone pain that doesn’t respond to typical stretching.
- A tendency to “brace” your belly all day or hold your breath during effort.
- Symptoms that worsen during high-stress weeks.
This is not a diagnostic list. It’s a pattern-recognition tool. If several of these fit, the most useful next step is an assessment with a qualified pelvic floor clinician.
Why Kegels are over-prescribed
Kegels are easy to explain and easy to “assign.” They also match a cultural bias: if something isn’t working, tighten and try harder. But pelvic health is more like learning a skill than building a single muscle. The best results come from restoring mobility, timing, and coordination—and then adding strength if needed.
- Doing Kegels without knowing whether you need them (or doing them when the pelvic floor is already overactive).
- Squeezing the wrong muscles (glutes, inner thighs, abs) and calling it a pelvic contraction.
- Training only “tighten,” never “release,” which reduces range of motion over time.
The fix starts with “drop before you lift”
If your pelvic floor runs tight, the first phase is often down-training: learning to relax and lengthen. This does not mean becoming “loose.” It means reclaiming full motion so the system can respond to load. Once range of motion returns, strengthening becomes more effective and less irritating.
The diaphragm and pelvic floor move together like a piston. On inhale, the pelvic floor should soften. Try “breathing into your underwear”: let the belly and low ribs expand, and imagine the pelvic floor gently widening on the inhale.
- Start with 2–3 minutes once or twice per day.
- Keep shoulders and jaw relaxed (they often mirror pelvic tension).
- If you feel “clenching” on inhale, reduce effort and slow down.
Instead of squeezing as if stopping urine, visualize the sit bones gently widening and the pelvic floor dropping down on inhale. Many high-achieving, high-stress people unconsciously brace their core and pelvis all day—this is the opposite practice.
For many people, learning to relax is the hardest strength skill they’ll ever practice.
Leaks often happen with pressure events: cough, laugh, jump, lift. A simple coordination cue is to exhale during effort. Exhale helps manage pressure and can improve timing—especially if you tend to hold your breath.
- Stand up from a chair: exhale as you rise.
- Lift a grocery bag: exhale as you pick it up.
- Cough/laugh: practice a gentle exhale with a soft “sss” sound.
When strengthening is the right move (and how to do it better)
If a clinician confirms that weakness or poor endurance is a primary issue, strengthening may be appropriate—but still not as “100 Kegels a day.” Effective strengthening is targeted, progressive, and paired with relaxation.
- Quality over quantity: fewer reps done correctly beat endless random squeezes.
- Train both: contract + fully release between reps.
- Include functional work: coordinate pelvic floor with real movements (squats, hinges, carries).
- Progress gradually: endurance first, then power/timing for impact activities.
See a specialist (why it’s worth it)
A pelvic floor PT can assess tone (too tight vs too lax), coordination, breathing patterns, and movement strategies—often using biofeedback to confirm what’s actually happening. Many people are surprised: they’ve been “doing Kegels” for years while contracting their glutes or holding their breath.
In some healthcare systems, postpartum pelvic rehab is routine; in others, women have to request it. If you have persistent symptoms, asking for a referral can be one of the highest-return health moves you make.
Red flags (don’t DIY these)
- Sudden severe pelvic pain, fever, or signs of infection.
- Blood in urine, severe burning, or recurrent urinary infections.
- New neurologic symptoms (numbness, weakness) or loss of bowel/bladder control.
- Significant prolapse symptoms (bulge sensation) or worsening heaviness.
- Pain with sex that persists or worsens despite rest and lubrication.
Practical next steps
- For 7 days, notice your default: are you bracing your belly or clenching your pelvis while sitting, driving, or working?
- Practice 2 minutes of diaphragmatic breathing daily with a gentle pelvic “drop” on inhale.
- Use “exhale on effort” for pressure moments (standing, lifting, coughing).
- If symptoms persist beyond a few weeks or interfere with life, request a referral to a pelvic floor PT for assessment.
- If you are postpartum, post-surgery, or have pain, prioritize professional guidance before doing aggressive strengthening.
Quick checklist
- I can fully relax my pelvic floor (not just contract it).
- I exhale on effort instead of breath-holding.
- My symptoms are improving or I have a plan for assessment.
- I’m not treating chronic pain or significant leakage as “normal.”
- I know when to seek clinical help rather than self-treat.
Important note: This article is educational and not medical advice. Pelvic floor symptoms have many possible causes. If you have significant pain, bleeding, infections, neurologic symptoms, or loss of bowel/bladder control, seek prompt medical evaluation. For persistent issues, a pelvic floor physical therapist or qualified clinician can guide an individualized plan.