This guide breaks down "I Thought I Needed TRT, I Just Needed Air": How Fixing My Sleep Cured My "Low T" into the key mechanisms and the decisions that matter in practice. By the time I turned 41, I felt like my batteries were permanently stuck at 15%. I was doing “the right things” on paper—lifting, eating fairly clean, trying a few supplements—and yet my body felt like it was running on fumes.
I didn’t feel sick in the classic way. I felt blunt. Flat mood, foggy focus, and a libido that had quietly disappeared. I assumed the culprit was hormonal aging. I was wrong. I had a breathing problem that was sabotaging every hormone downstream.
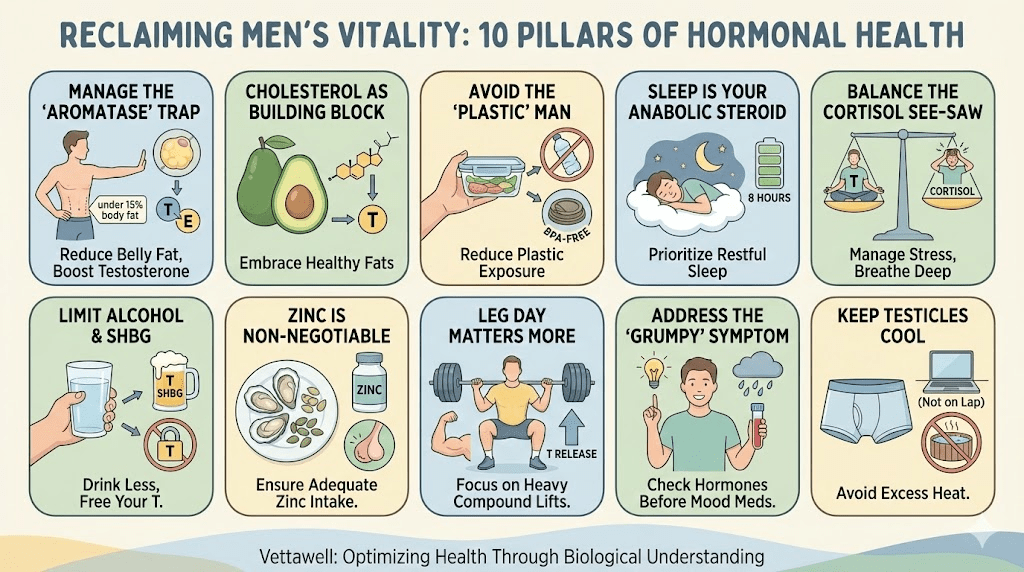
Key takeaways
- Low testosterone symptoms can be secondary to disrupted sleep architecture, not primary testicular failure.
- A high hematocrit (or rising hemoglobin) can be a clue for chronic nighttime hypoxia and makes “quick TRT” riskier.
- Obstructive sleep apnea fragments REM and deep sleep, amplifies cortisol, and can flatten libido, mood, and body composition.
- The fastest “upgrade” for many men is not a new supplement stack—it’s restoring airflow and stable oxygen at night.
“I’m not giving you testosterone. If you’re suffocating at night, the first prescription is oxygen.”
The Symptom Stack
Looking back, the clues were obvious. I just didn’t know how to interpret them. My issues weren’t isolated—they were a cluster that all pointed to the same root problem: chronic sleep fragmentation.
- Morning hangover without drinking: waking up groggy, dry-mouthed, and needing caffeine immediately.
- Brain fog + short fuse: reading the same email twice, snapping at small stressors, feeling “wired but tired.”
- Stubborn belly gain: especially around the midsection, despite training consistency.
- Libido collapse: not just performance, but interest—as if the switch had been turned off.
- Loud snoring + gasping: reported by a partner, plus waking to pee (nocturia) more than expected.
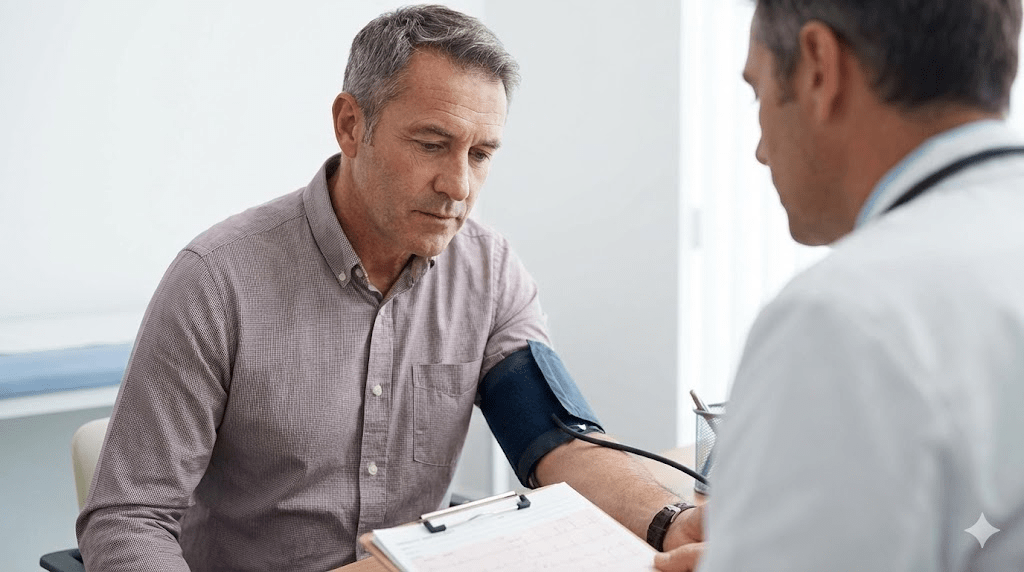
The Clinic Visit I Thought Would End in TRT
I walked into a men’s clinic with a script in my head: “Low T, please fix.” The doctor did what a good clinician does—he didn’t just look at total testosterone and stop there. He scanned the broader risk picture.
My Total Testosterone came back at 320 ng/dL—“low-normal.” Not great, but not the disaster I expected. Then he paused at my hematocrit. It was unusually high for someone who wasn’t on TRT.
That’s when he asked the question that changed the story: “Do you snore?” I laughed. My wife didn’t. She had been complaining for years.
Why Hematocrit Was the Red Flag
High hematocrit can have multiple causes, but one common pathway is simple physiology: when the body senses low oxygen (especially during sleep), it compensates by producing more red blood cells to carry oxygen. In other words, the blood thickens to survive the shortage.
- The hidden risk: TRT can further increase hematocrit in some men, raising clot/stroke risk if the baseline is already elevated.
- The real clue: a “blood problem” was pointing to an “air problem.”
The Diagnosis: Moderate Sleep Apnea
I agreed to a home sleep study thinking it would be a formality. It wasn’t. My AHI (Apnea–Hypopnea Index) was 26—meaning 26 breathing interruptions per hour. That’s roughly one event every two to three minutes.
The scary part wasn’t just the interruptions. It was what they caused: repeated micro-arousals, repeated stress-hormone spikes, and repeated dips in oxygen that trained my nervous system to live in “threat mode.”
How Sleep Apnea Lowers Testosterone (Without Touching the Testes)
Most men think testosterone is purely a “gonads” issue. In reality, testosterone is a sleep-governed hormone. The brain needs consolidated sleep—especially deep sleep and REM—to run the endocrine repair cycle.
- Fragmented REM: apneas trigger micro-wake-ups that cut REM into tiny fragments. Testosterone production and libido signaling suffer.
- Chronic sympathetic activation: every oxygen dip triggers an adrenaline response; cortisol rises and stays elevated.
- Insulin resistance pressure: poor sleep drives glucose volatility, which increases visceral fat and further worsens airway collapse.
- The vicious loop: more visceral fat → narrower airway → worse apnea → worse hormones → easier fat gain.
The Counter-Intuitive Truth
I wasn’t “aging badly.” I was under-oxygenated and chronically sleep-deprived. And because the impairment is gradual, you normalize it. You forget what “fully rested” feels like, so you assume your new baseline is just adulthood.
The Protocol: Oxygen First, Then Everything Else
We didn’t touch TRT. We treated airflow and sleep architecture like the primary system—and everything else like a downstream variable. The plan had three layers: medical therapy, positional mechanics, and behavioral triggers.
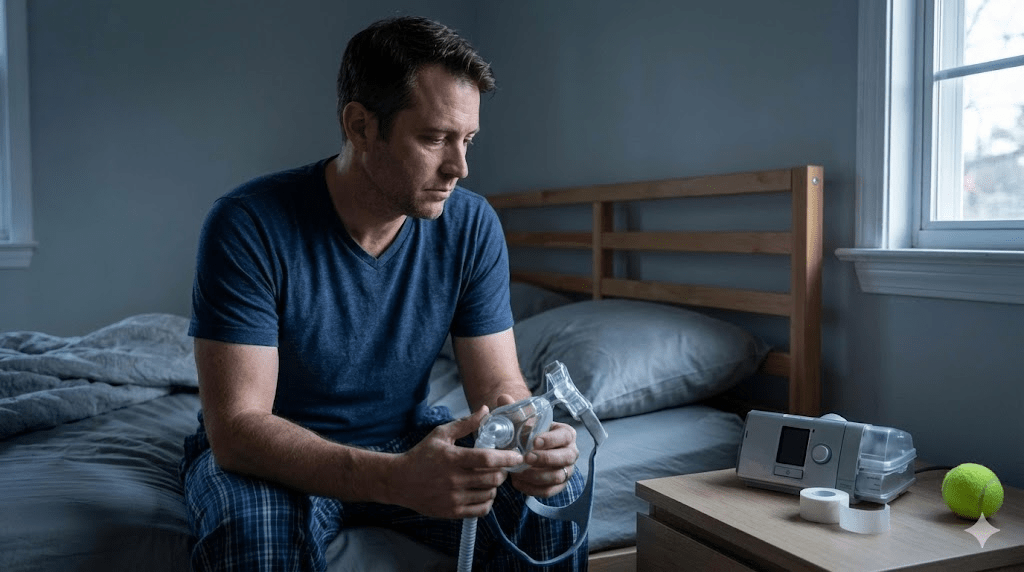
1) CPAP (The Unsexy Fix That Works)
CPAP felt like admitting defeat. It turned out to be the most effective performance upgrade I’ve ever used. The first night was awkward. The second night, I slept seven hours straight. The next morning I had something I hadn’t felt in years: steady alertness.
- Make it stick: use humidification if your nose dries out; try different masks; optimize strap tension; don’t quit after two nights.
- Track the data: most modern CPAP devices report leak rate and residual AHI. Small adjustments can make a big difference.
2) Positional Therapy (Side-Sleeping as a Mechanical Hack)
My apnea was worse on my back. Gravity collapses the airway; the tongue and soft tissue fall posteriorly. I used a crude trick—sewing a tennis ball into an old T-shirt—to keep myself from rolling supine.
- What it does: reduces back-sleeping, which can substantially lower events for position-dependent apnea.
- Bonus: side-sleeping often reduces snoring intensity, which improves partner sleep and relationship strain.
3) Nasal Breathing and the Mouth-Taping Caveat
I was a habitual mouth-breather. Nasal breathing tends to promote calmer autonomic tone and can reduce dryness and snoring in some people. I experimented with a small strip of gentle tape as a reminder to keep my lips closed.
- Important safety note: mouth taping is not for everyone. Do not tape if you have nasal obstruction, chronic congestion, panic around breathing, reflux-related choking, heavy alcohol use, or suspected severe apnea without medical supervision.
- Safer alternatives: nasal strips, saline rinse, treating allergies, or simply practicing daytime nasal breathing to reduce mouth-breathing habits.
Behavioral Moves That Made the Medical Treatment Work Better
Apnea is structural, but it’s also sensitive to certain triggers. I didn’t need perfection—just a few leverage points that reduced nighttime airway instability.
- Alcohol cut-off: alcohol relaxes airway muscles; I avoided it within 3–4 hours of bed.
- Late meal reduction: heavy meals close to bedtime worsened reflux and breathing quality.
- Consistent sleep window: I stopped treating bedtime like an optional suggestion.
- Weight-neutral focus: even modest reductions in visceral fat can improve airway mechanics, but the first win was oxygen—not dieting.
The Outcome
After three months, I repeated blood work. I hadn’t redesigned my diet. I hadn’t changed my workout split. The only major change was sleeping with stable airflow. My Total Testosterone rose from 320 to 680 ng/dL.
The secondary effects were just as meaningful: my belly started shrinking, my mood stabilized, and the “old man in a young man’s body” feeling disappeared. My wife slept through the night too—an underrated benefit that made the whole house calmer.
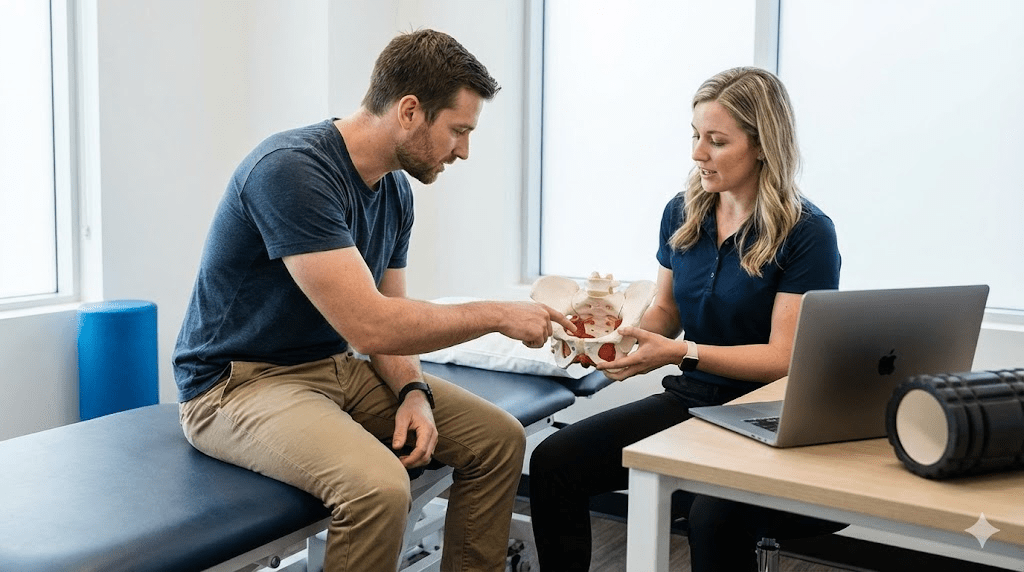
What to ask your doctor for
- Sleep evaluation: home sleep test or in-lab study if symptoms suggest apnea.
- Full hormone picture: total T + free T (or calculated), SHBG, LH/FSH (to distinguish primary vs secondary hypogonadism).
- Cardiometabolic markers: fasting glucose/insulin, A1c, lipids, blood pressure.
- CBC trend: hemoglobin/hematocrit monitoring, especially if considering TRT.
Practical next steps
- If you snore, wake up unrefreshed, or have daytime sleepiness, treat sleep as a medical system—not a lifestyle preference.
- Address airflow first (evaluation + therapy) before escalating to hormone replacement.
- Keep training, but prioritize recovery: consistent sleep timing and low evening stress load.
Common pitfalls
- Chasing TRT as a first-line fix without investigating apnea, especially when hematocrit is high.
- Assuming “I’m asleep for 6 hours” equals recovery—micro-arousals can destroy sleep quality without your awareness.
- Using alcohol or sedatives to force unconsciousness, which can worsen breathing events and next-day hormones.
- Quitting CPAP too early due to discomfort before doing basic fit and humidity troubleshooting.
Quick checklist
- Partner reports snoring, gasping, or witnessed pauses in breathing.
- Morning headaches or dry mouth are reduced.
- Energy is stable through the afternoon without escalating caffeine.
- Libido and mood are improving over weeks, not hours.
- If using CPAP, residual AHI and leak rates are trending in the right direction.