Mark, a 32-year-old software developer, remembers exactly when the pain started—not because something dramatic happened, but because it didn’t. There was no injury, no risky weekend, no obvious trigger. Just a dull ache in the perineum (the area between the scrotum and anus) that slowly evolved into burning during urination and a constant sensation that he was sitting on a golf ball.
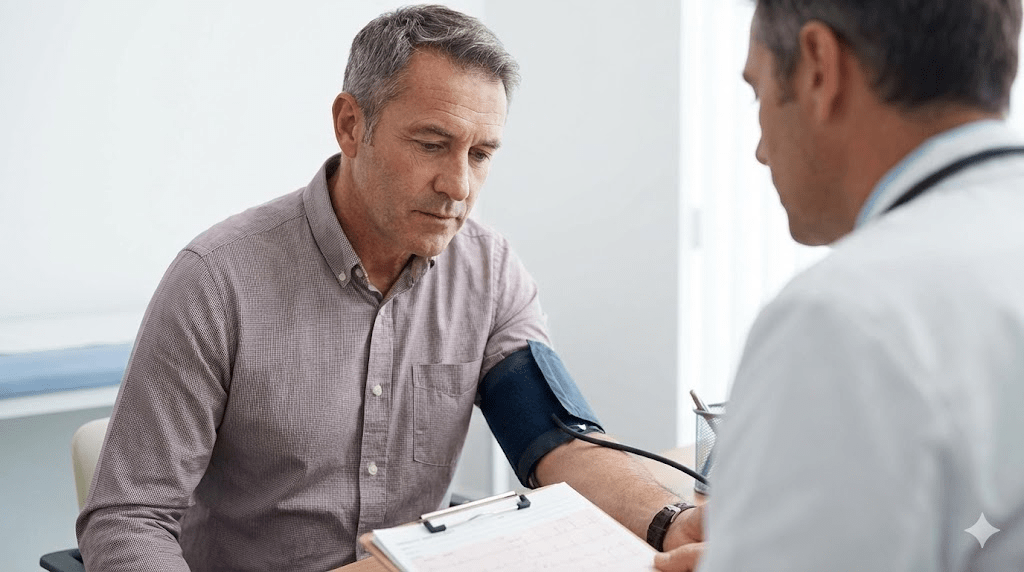
He did what most men do when something feels wrong “down there”: he assumed it had to be an infection. The system agreed. The first urologist labeled it prostatitis and sent him home with a 30-day course of antibiotics. When the pain didn’t improve, he received another course. Tests kept coming back negative, yet the symptoms remained—and Mark’s anxiety surged.
The most terrifying part wasn’t the pain. It was the feeling that nobody could explain it.
Key takeaways
- Many cases labeled “prostatitis” are not bacterial infections—they’re neuromuscular pain syndromes.
- Chronic pelvic pain can be driven by a hypertonic (overactive) pelvic floor, stress physiology, and sitting-related compression.
- Antibiotics can’t fix a muscle cramp, nerve irritation, or central sensitization—so symptoms persist even when tests are negative.
- Recovery often requires a different playbook: down-training tension, restoring hip/core mechanics, and retraining safety signals in the nervous system.
- The goal is not “tightening” the pelvic floor, but regaining range of motion + control.
What Mark thought was happening
Mark’s symptoms looked like a urology problem: urinary burning, pelvic heaviness, urgency, discomfort after sitting. He also noticed the pain spiked during deadlines and eased slightly on weekends—until the anxiety made weekends feel like “recovery shifts” instead of rest.
When you’re in pain in a private area, the brain hunts for a simple, concrete explanation. Infection is psychologically tidy: you find a germ, you kill it, you move on. But Mark’s repeated negative cultures created a mismatch: the tests said “no bacteria,” but his nervous system kept yelling “danger.”
If the driver is muscular guarding, nerve sensitivity, or a pain-signal loop, antibiotics may do nothing. Worse, repeated courses can reinforce the belief that something is “still there,” amplifying hypervigilance and tension—which feeds the symptoms.
When pain becomes chronic, the question shifts from “What pathogen is causing this?” to “What system is stuck in protection mode?”
The "Headache in the Pelvis"
What Mark had instead was consistent with CPPS (Chronic Pelvic Pain Syndrome)—often described as a “headache in the pelvis.” It’s not a single disease. It’s a pattern: pelvic muscles stay tense, nerves become irritated, and the brain learns the pain signal until it becomes automatic.
Just as some people clench their jaw during stress, many men clench their pelvic floor without realizing it—especially during intense concentration. In software terms, Mark was running a background process all day: brace → guard → tighten → amplify.
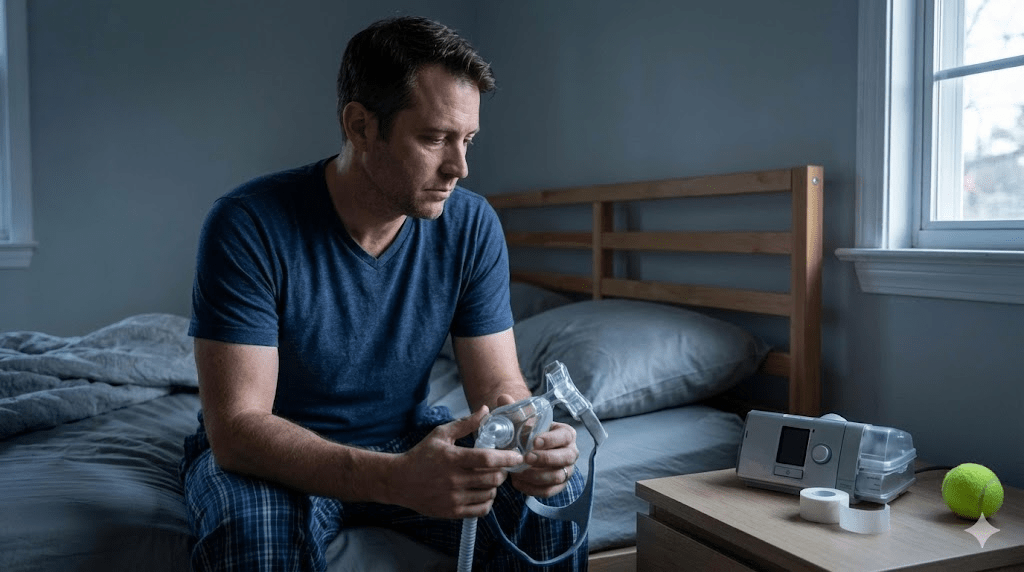
- Sedentary compression: sitting for hours can irritate pelvic nerves and reinforce muscle guarding.
- Stress physiology: high arousal states increase muscle tone and reduce the body’s ability to downshift into recovery.
Mark also had a habit common in high-pressure environments: “sucking in” his stomach to look leaner. That constant abdominal bracing can force the pelvic floor to compensate—like a foundation carrying weight it wasn’t designed to hold all day.
- Discomfort appears → you tense in response (often unconsciously).
- Tension reduces blood flow + increases nerve irritation.
- Irritation increases symptoms (burning, urgency, “golf ball” pressure).
- Symptoms trigger more vigilance (“What if it’s serious?”).
- Vigilance increases stress arousal → pelvic muscles tighten again.
Signs it might be pelvic-floor driven, not infectious
Only a clinician can diagnose causes of pelvic pain, but certain patterns often point toward a neuromuscular driver—especially when labs are repeatedly normal.
- Symptoms fluctuate with stress, posture, or long sitting sessions.
- Pain improves temporarily with heat, movement, or relaxation.
- Urinary tests are negative and antibiotics change little.
- Hip tightness, glute weakness, or lower back stiffness coexist.
- There’s a sense of “clenching” or bracing during focus or anxiety.
If you can turn symptoms up with stress and down with release, you’re often looking at a nervous-system and muscle-control problem.
The turning point
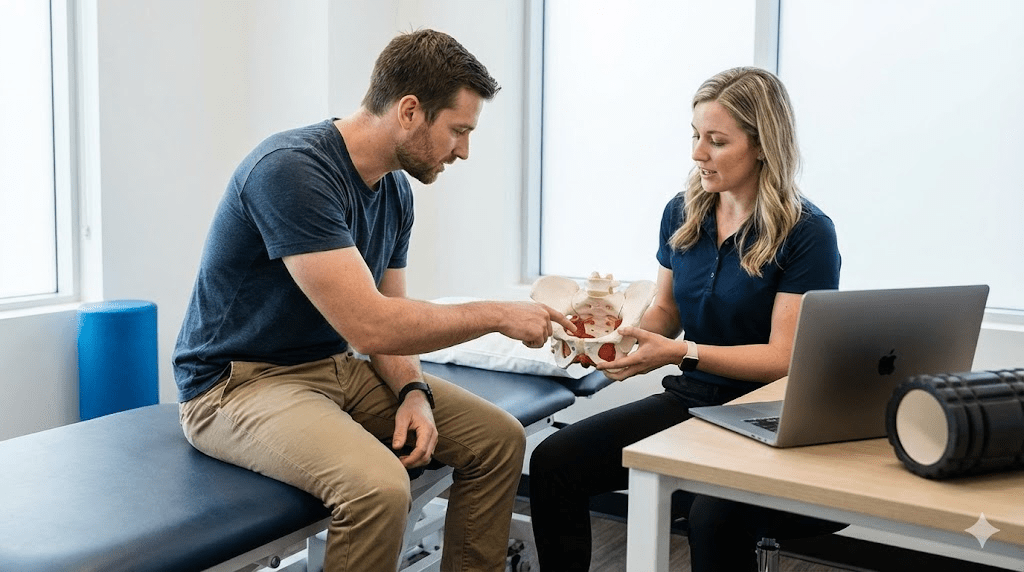
Mark eventually found a physical therapist specializing in male pelvic health. She didn’t begin with his prostate. She began with his breathing, posture, hips, and core control.
Her summary was blunt: “Your pelvic floor is frozen in a panic state.” His glutes weren’t doing their job, his hips were stiff, his diaphragm mechanics were shallow, and his default under pressure was to clamp down. The target wasn’t strength—it was range, coordination, and safety.
Mark had been doing Kegels (squeezing) because he assumed pelvic symptoms meant weakness. For many men with CPPS patterns, that’s like trying to fix a tight neck by shrugging harder. The first move was the opposite.
Drop, don’t squeeze.
Mark’s recovery protocol
His plan wasn’t a single exercise. It was a system for unwinding tension, restoring mechanics, and training the nervous system to stop treating normal sensations as emergencies.
- Diaphragmatic breathing: slow nasal inhale, long exhale; letting the belly soften instead of bracing.
- Reverse Kegel cueing: visualizing the pelvic floor widening and lowering on inhale (no forced pushing).
- Heat + gentle mobility: warm baths or heat packs followed by slow hip-opening movements to reduce guarding.
The therapist focused on hips and pelvic mechanics—areas that often become stiff when you sit and brace for years.
- "Happy Baby" pose: 5–10 minutes daily, gently encouraging pelvic floor lengthening.
- Hip flexor and adductor release: short, consistent sessions rather than aggressive stretching.
- Glute activation basics: rebuilding support so the pelvic floor stops trying to do every job.
Mark’s symptoms flared during coding sprints, conflict, and deadlines. So he trained a “check-in reflex” to catch tension early—before it became pain.
- Set a timer every 60–90 minutes during work.
- Scan: jaw, shoulders, belly, pelvic floor—notice clenching without judgment.
- Exhale longer than you inhale for 5 breaths.
- Stand, walk 2 minutes, then return to work.
For some people, internal trigger points are part of the picture. Mark’s therapist explained that internal muscles can develop knots that refer pain outward. In his case, hands-on therapy was introduced carefully and progressively.
- This is not a DIY first step; it should be taught by a qualified pelvic health clinician.
- The goal is gentle release and desensitization—never force, never pain-chase.
- If symptoms worsen significantly, the plan gets adjusted (more down-training, less intensity).
What improved first—and what took time
Mark didn’t wake up cured after one stretch. But he did notice early wins that proved the diagnosis finally fit: the “golf ball” sensation softened after breathing and movement; flare-ups became shorter; sitting was less provocative.
- First 2 weeks: better awareness of clenching, fewer end-of-day spikes, less catastrophic thinking.
- Weeks 3–8: longer symptom-free windows, reduced urinary urgency, improved tolerance for sitting.
- Months 3–4: burning largely resolved, pain no longer governed decisions, flare-ups became manageable and predictable.
The outcome
After four months of consistent work, the “golf ball” sensation vanished. The burning stopped. Mark became pain-free—not because he found the right pill, but because he stopped treating a neuromuscular problem like a bacterial one.
He now treats pelvic health like oral hygiene: regular movement breaks, hip mobility, stress downshifts, and a standing desk. The lesson that stuck wasn’t “stretch more.” It was: my body was sending a signal that my stress-and-sitting lifestyle was unsustainable.
He didn’t need stronger antibiotics. He needed permission—and a plan—to let go.
Practical next steps
- Rule out red flags with a clinician (fever, blood in urine, acute urinary retention, severe new pain).
- If tests are negative and symptoms persist, ask about male pelvic floor physical therapy and CPPS evaluation.
- Start with down-training: 5 minutes of slow breathing + pelvic relaxation cues daily.
- Reduce sitting pressure: stand/walk for 2 minutes every hour; try a cushion if needed.
- Strengthen support: basic glute + core coordination work (guided if possible).
- Track triggers (stress, sitting, workouts) to predict and shorten flare-ups.
Common pitfalls
- Assuming ongoing symptoms mean “missed infection” despite repeated negative testing.
- Doing high-volume Kegels or aggressive core bracing that increases pelvic tension.
- Pain-chasing with intense stretching instead of consistent, gentle release.
- Ignoring stress physiology—treating it as “mental” rather than biological muscle tone.
- Trying advanced internal techniques without professional instruction.
Important note: This article is educational and not medical advice. Pelvic pain can have multiple causes. If you have persistent symptoms, consult a qualified healthcare professional for diagnosis and treatment.