Most men don’t wake up one day with a dramatic “low testosterone” sign. They wake up with subtle degradation: a shorter fuse, a softer waistline, lower drive, worse sleep, and workouts that feel harder for less return. The mistake is treating this like a motivation problem. It’s usually a systems problem—sleep, stress, body composition, fueling, and environment shaping the endocrine axis over time.
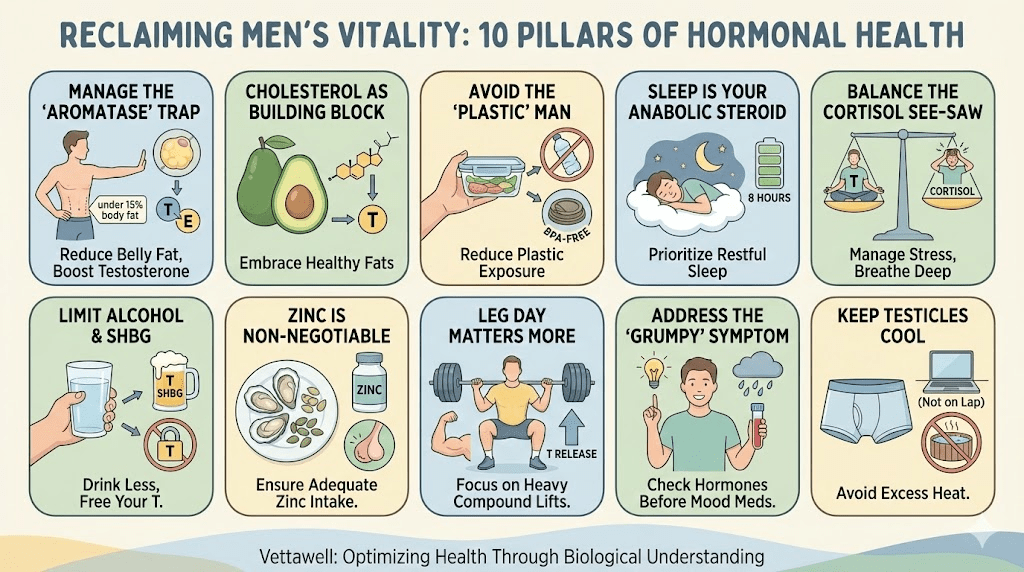
Testosterone matters, but it’s not a single dial you “turn up.” It’s a network: brain (hypothalamus/pituitary), testes, liver (SHBG), fat tissue (aromatase), and the nervous system. When the system is under chronic load, men often feel tired before they see classic sexual symptoms. The good news: most drivers are modifiable.
If you’re tired all the time, don’t start with a “booster.” Start by asking: what is my body protecting me from right now?
Key takeaways
- Hormones respond to inputs (sleep, stress, nutrition), outputs (training load, recovery), and storage (visceral fat).
- “Low T” is not always low production—it can be low free testosterone (high SHBG) or high conversion to estrogen (high aromatase).
- The fastest sustainable wins usually come from: better sleep regularity, resistance training, waist reduction, and less alcohol.
- A smart plan starts with measurement: Total T + Free T + SHBG, plus cardiometabolic markers and thyroid basics.
Before you change anything: measure the right things
Men often chase symptoms (fatigue, low libido, low motivation) without checking the underlying signals. A basic “total testosterone” number is not the full story. For many men, total T is borderline-normal while free T is low because it’s being bound up.
- Core hormone context: Total testosterone, Free testosterone (or calculated), SHBG.
- Axis check: LH and FSH (help distinguish production vs. signaling).
- Red flags to rule out: Prolactin, thyroid (TSH ± Free T4), ferritin/iron status if fatigue is significant.
- Metabolic context: fasting glucose/insulin, A1c, triglycerides, HDL, blood pressure, waist circumference.
If you have severe symptoms, infertility concerns, or sudden changes, work with a clinician. Hormone therapy can be appropriate for some men, but lifestyle drivers often determine whether any intervention works—or backfires.
The 10 biological truths
Visceral fat acts like an endocrine organ. It produces inflammatory signals and increases aromatase, an enzyme that converts testosterone into estradiol. The result can be a double hit: lower effective androgens and higher estrogenic signaling, which often shows up as fatigue, low drive, and stubborn midsection gain.
- What to do: Treat waist size like a health metric, not a vanity metric. Prioritize daily walking, protein-forward meals, and resistance training.
- Practical benchmark: Aim for a steady reduction in waist circumference over “scale drama.” Visceral fat often moves first when the plan is consistent.
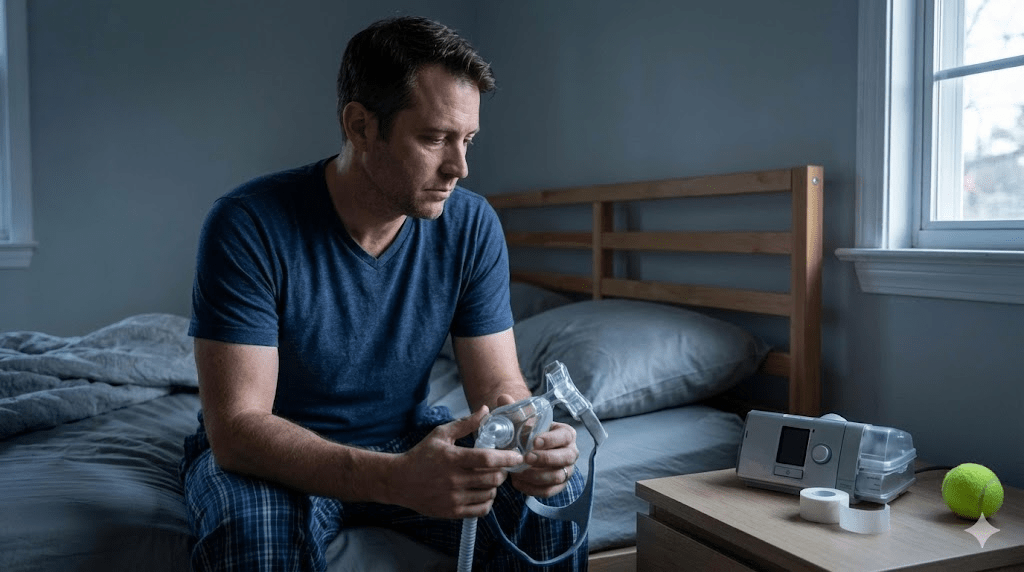
A major share of daily testosterone secretion is tied to sleep quality and continuity. When sleep is short, fragmented, or misaligned (late-night screens, alcohol, irregular wake times), the endocrine system shifts toward stress hormones and away from anabolic repair.
- Sleep anchor: set a consistent wake time (even weekends).
- Protect deep sleep: cool, dark room; no heavy meals late; reduce alcohol; wind-down buffer.
- If you snore loudly or wake up choking: consider screening for sleep apnea—untreated apnea can crush energy and hormones.
You can’t out-supplement a nervous system that never gets to recover.
Cortisol and testosterone behave like a seesaw. Acute stress is normal; chronic stress is endocrine sabotage. Over time, constant “on” mode can reduce gonadotropin signaling (LH/FSH) and shift resources toward survival.
- Downshift tool: two short inhales + one long exhale (physiological sigh) when arousal spikes.
- Boundary rule: a real “off” window most days (no work messages).
- Training implication: when life stress is high, reduce intensity before you reduce consistency.
If you combine high training load with fasting or chronically low calories, the body often down-regulates reproduction. Men can maintain aesthetics while endocrine signals deteriorate—low libido, poor sleep, irritability, and plateaued performance.
- What to do: fuel training. Most men do better with protein at breakfast and carbohydrates around workouts (timing matters).
- Watch the signals: cold hands/feet, persistent soreness, low morning energy, and loss of morning erections can be “under-recovery” clues.
Steroid hormones are synthesized from cholesterol. Extreme low-fat diets can leave the body short on building blocks, especially when combined with high stress and high training. This doesn’t mean “eat junk fats.” It means don’t starve the endocrine system of essentials.
- Build with quality: whole eggs, olive oil, fatty fish, nuts/seeds, avocados.
- Avoid the trap: replacing fat with ultra-processed “low-fat” foods often worsens metabolic markers.
Alcohol doesn’t only affect the liver; it affects sleep architecture, insulin sensitivity, and sex hormone binding. Some men see normal total testosterone on labs but feel symptoms because free T is reduced (often via higher SHBG), and sleep quality is impaired.
- Simplest upgrade: reduce frequency before you argue about “type of alcohol.”
- If you drink: keep it earlier, keep it smaller, and avoid pairing it with late-night eating—sleep and glucose take the biggest hit.
Modern life increases exposure to chemicals that can interfere with hormone signaling (often referred to as endocrine disruptors). You don’t need to live in a bunker, but small swaps reduce chronic exposure.
- High-impact swaps: don’t microwave food in plastic; use glass/stainless for hot liquids; store leftovers in glass.
- Personal care: reduce heavy fragrance products if you’re sensitive; choose simpler formulations when possible.
Your endocrine system responds to mechanical load. Heavy compound movements recruit large muscle groups and improve insulin sensitivity—both supportive of healthier testosterone dynamics over time. But the goal is adaptation, not annihilation.
- Best ROI movements: squats/hinges (or variations), presses, rows, loaded carries.
- Dose: 3–4 strength sessions/week beats 6–7 “grind” sessions you can’t recover from.
- Don’t skip Zone 2: steady cardio supports mitochondria and metabolic health, which often improves hormonal symptoms indirectly.
The best training plan is the one you can recover from consistently.
Many over-the-counter “boosters” are expensive noise. Basic deficiencies—especially zinc, magnesium, vitamin D, and omega-3 intake—can meaningfully affect energy, sleep, and endocrine signaling. Food-first usually wins.
- Zinc sources: oysters, beef, pumpkin seeds (supplement only if needed).
- Vitamin D: sunlight + testing if symptoms are persistent or you live indoors most of the year.
- Magnesium: supports sleep quality and stress tolerance; food sources include leafy greens, nuts, and legumes.
Sperm and testosterone production require cooler temperatures than core body heat. Chronic heat exposure (long hot baths, frequent saunas without recovery, laptop-on-lap habits, tight non-breathable clothing) can reduce function—especially relevant for fertility.
- Easy fixes: keep laptops off your lap; choose breathable underwear; avoid prolonged heat when trying to conceive.
- Context matters: heat exposure isn’t “bad,” but chronic + combined stressors can tip the system.
A simple 14-day reset that doesn’t rely on supplements
If you want a clean experiment, run a two-week protocol focused on the highest-leverage levers. Don’t change ten things at once. Track energy, sleep, libido, morning mood, and training performance.
- Anchor wake time: same wake time daily; aim for 7–9 hours in bed.
- Protein-first breakfast: within 60–90 minutes of waking; keep it savory.
- Daily movement: 30–60 minutes walking (can be broken into chunks).
- Strength 3x/week: compound-focused, stop 1–2 reps before failure.
- Alcohol pause (or major reduction): observe what changes in sleep and mood.
- Evening buffer: 60 minutes pre-sleep with dim lights and no work screens.
Practical next steps
- Treat symptoms as signals: check cardiometabolic risk markers alongside hormones (waist, BP, lipids, glucose).
- Prioritize sleep quality and regularity for 14 days before adding new supplements.
- Build muscle with consistent resistance training, then adjust nutrition to support it.
- If symptoms persist, get a full panel (Total T, Free T, SHBG, LH/FSH) and review with a clinician.
Common pitfalls
- Chasing a “magic booster” while sleep, alcohol, and stress remain unchanged.
- Overtraining + under-fueling (especially with frequent fasting) and calling the crash “aging.”
- Looking only at Total T and ignoring Free T / SHBG context.
- Treating mood and motivation symptoms as purely psychological without checking physiology.