Jason, a 45-year-old project manager, spent three weeks working up the courage to make the appointment. He wasn’t “unhealthy,” exactly. He didn’t smoke, played golf on weekends, and told himself his desk job was balanced out by a few bursts of activity.
But recently, things in the bedroom had become unreliable. He blamed deadlines, stress, and getting older. He walked into his doctor’s office with a rehearsed speech and a simple request: a quick prescription and a quick return to normal.
“I just need the blue pill, Doc. Just something to get me back in the game.”
Jason expected a five-minute visit. Instead, his doctor put down the pen and picked up a blood pressure cuff. “We can talk about medication,” the doctor said, “but first I need to understand why your blood flow is failing. Because if it’s failing there, it may be failing elsewhere too.”
Key takeaways
- For many men over 40, erectile dysfunction (ED) is often linked to vascular health, not “motivation” or masculinity.
- Because penile arteries are small, ED can appear years before other cardiovascular symptoms in some men.
- PDE5 inhibitors (the “blue pill” category) can improve function, but they do not automatically address underlying drivers like blood pressure, insulin resistance, lipids, or endothelial dysfunction.
- The most useful first step is not shame—it’s evaluation: blood pressure, metabolic markers, and a cardiovascular risk conversation.
- You can often improve blood flow by improving the systems that create it: sleep, activity, nutrition, and stress physiology.
The canary in the coal mine
Jason didn’t know that ED is rarely “just a bedroom problem.” In many cases, it’s a blood vessel problem. Erections are a vascular event: they depend on healthy arteries, responsive smooth muscle, and a nervous system that can shift into a relaxed, parasympathetic state.
There’s a practical reason ED can show up early. The arteries supplying the penis are small—often described as roughly 1–2 mm wide—while coronary arteries feeding the heart are larger. When plaque begins to develop or the vessel lining becomes dysfunctional, the smallest “pipes” can show reduced flow first. For some men, ED appears 2–5 years before heart attacks or other cardiovascular events.
ED can be a “check engine light.” Not every light means disaster—but every light deserves attention.
- It does mean: ED is a reason to discuss cardiovascular risk and metabolic health, especially after 40.
- It does not mean: ED guarantees a heart attack is coming. Many causes exist (psychological, medication-related, hormonal, neurologic).
- The point: treat ED as a signal worth investigating, not a secret to hide.
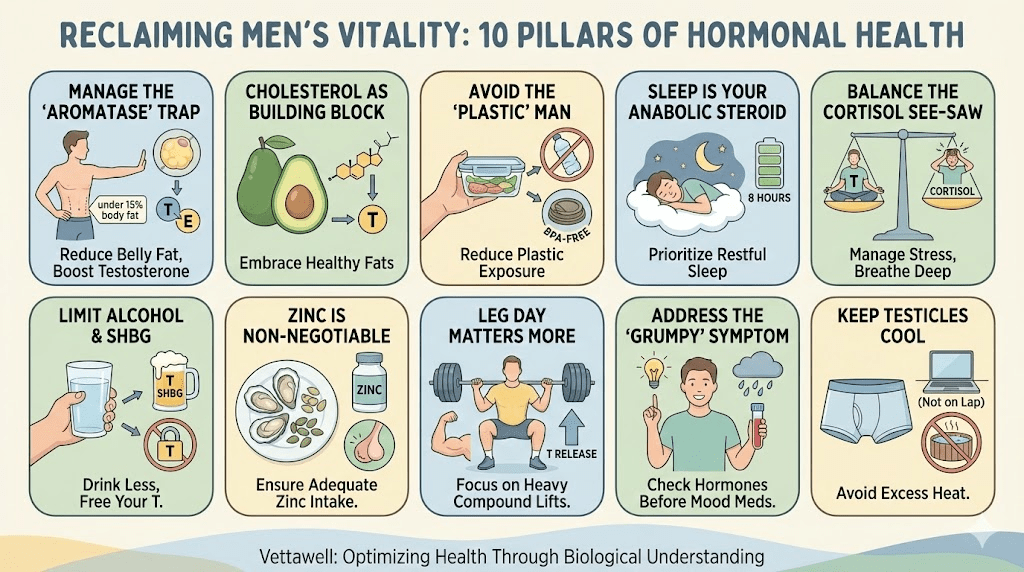
It’s not always low T. Often it’s low NO.
Jason assumed testosterone was the likely culprit. But his bloodwork told a different story. Testosterone was within range. The issues were elsewhere: blood pressure trending high, LDL elevated, triglycerides up, fasting glucose creeping, and inflammatory markers not great.
The doctor explained the mechanism in plain English: the lining of your blood vessels (the endothelium) produces nitric oxide (NO)—a key signal that tells arteries to relax and open. When endothelial function declines, arteries become less responsive. Less NO means less vasodilation. That affects the whole body, including erections.
Medications like sildenafil or tadalafil (PDE5 inhibitors) support erections by enhancing the NO–cGMP pathway in smooth muscle, making it easier for blood vessels in penile tissue to relax in response to sexual stimulation. They can be effective—but they’re not a vascular rehabilitation plan. They amplify a pathway; they don’t automatically repair the vessel wall.
The hidden drivers Jason recognized in himself
When the doctor asked about Jason’s week, the pattern was familiar: sedentary workdays, processed lunches, irregular sleep, and “exercise” that was mostly occasional bursts. Nothing looked catastrophic. But the cumulative effect was predictable.
- Sitting + low daily movement: less shear stress on vessels, less endothelial stimulus.
- Ultra-processed meals: higher glycemic load and lipid burden, often paired with low fiber.
- Sleep debt: worsens insulin sensitivity and increases sympathetic tone.
- Chronic stress: keeps the nervous system in “performance mode,” which competes with sexual function.
- Alcohol as a coping tool: can blunt sleep quality and impair erectile physiology.
The “save your life” protocol (the deal)
Jason’s doctor didn’t moralize. He offered a deal: yes, he would consider prescribing a PDE5 inhibitor after basic screening—and Jason would treat this as a cardiovascular warning flare. The goal wasn’t to scare him; it was to use the signal while there was still time to change the trajectory.
“We’re not treating a moment. We’re treating the system that produces the moment.”
The doctor laid out a simple list: “If your blood flow is struggling, we need to see the usual suspects.”
- Blood pressure: in-office and home readings (trend matters more than one number).
- Lipids: LDL, HDL, triglycerides (and sometimes ApoB / Lp(a) depending on risk).
- Glycemic status: fasting glucose and HbA1c (sometimes fasting insulin).
- Body composition: waist circumference and strength/endurance baselines.
- Sleep and stress: because physiology doesn’t compartmentalize.
Jason didn’t need a trendy diet. He needed consistent inputs that improved endothelial function: fiber, micronutrients, protein, and fewer processed calories. The doctor emphasized nitrate-rich foods as one supportive lever—especially from vegetables.
- Beets, arugula, spinach: natural dietary nitrates that can support NO availability in the body.
- Citrus + leafy greens: vitamin C and polyphenols that support vascular function.
- High-fiber carbs: legumes, oats, berries—better glycemic stability than refined starch.
- Omega-3 sources: fatty fish, walnuts, flax (as part of a broader plan).
Jason expected nutrition advice. He didn’t expect microbiome advice. The doctor explained that certain oral bacteria help convert dietary nitrates into forms that can support NO production. Overusing antiseptic mouthwash may reduce this conversion in some people. The takeaway wasn’t “never use mouthwash,” but “don’t assume the strongest antiseptic option is always neutral.”
Zone 2 cardio: the endothelial rehab session
Jason was relieved when the exercise prescription was not “crush yourself.” He was told to build a base: steady, conversational cardiovascular training—often called Zone 2. The logic is simple: consistent low-to-moderate work improves vascular function and metabolic flexibility without the recovery cost of constant maximal effort.
- 3 sessions per week, 25–40 minutes each (walking incline, cycling, rowing—whatever is sustainable).
- Intensity: you can talk in sentences, but you’re clearly working.
- Bonus: walk the golf course instead of riding the cart when possible.
Strength training: the insulin and testosterone ally
Cardio improves the pipes. Strength training builds the engine. Muscle tissue supports glucose disposal and improves insulin sensitivity, both of which affect vascular health. Jason didn’t need bodybuilding—he needed consistent resistance training that made him stronger over time.
- Two full-body strength sessions per week to start.
- Focus on compound patterns: squat/hinge/push/pull/carry (scaled to ability).
- Progress slowly; avoid the “weekend warrior” injury cycle.
- Pair it with protein at meals to support recovery and lean mass.
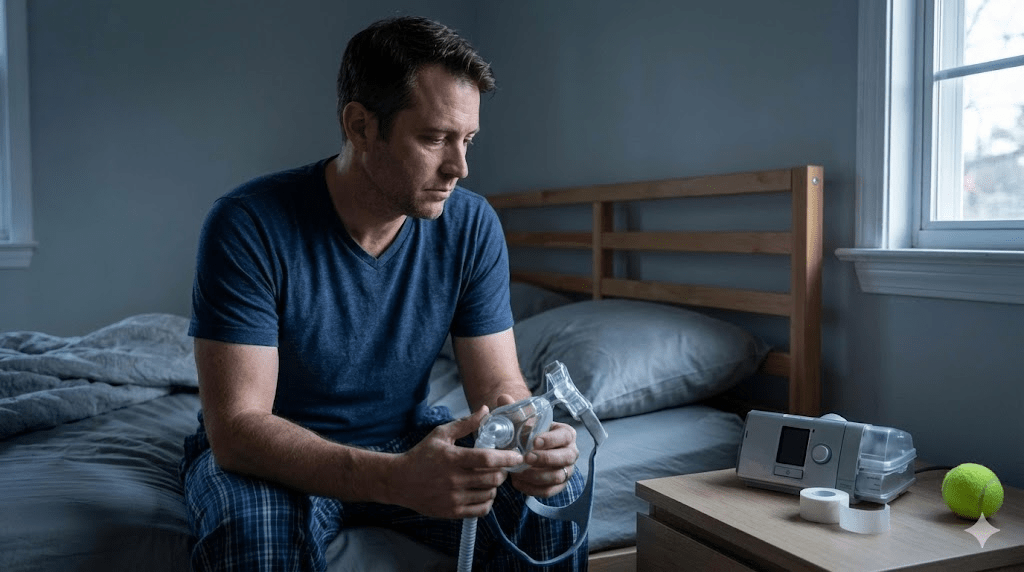
Sleep: where hormones and NO get replenished
Jason’s doctor was blunt: “You can’t out-supplement poor sleep.” Deep sleep supports hormone regulation, vascular recovery, and nervous system balance. Late-night scrolling and inconsistent bedtimes were quietly sabotaging him.
- A consistent wake time (even on weekends, within ~60 minutes).
- A screen-off buffer to allow downshifting before bed.
- Less alcohol, especially late—because sedation isn’t the same as recovery.
What Jason changed in 30 days
Jason didn’t transform overnight. He didn’t need to. The first month was about consistency and metrics, not motivation. His changes were intentionally boring—the kind that actually stick.
- Walked 10 minutes after lunch most days (blood sugar and stress both improved).
- Swapped his default lunch for a protein + fiber plate 4 days per week.
- Added 3 Zone 2 sessions weekly and 2 strength sessions.
- Moved caffeine earlier and created a real wind-down routine.
The fastest improvements came from the basics—not from hacks.
The outcome (and why it mattered)
Six months later, Jason’s blood pressure was down, his waist measurement improved, and his lipid profile moved in the right direction. His energy was better. His sleep was more stable. And yes—his sexual function improved enough that he used medication less often, and in some periods not at all.
The surprising part wasn’t the bedroom win. It was the mindset shift: what felt like an embarrassing problem turned into a meaningful early warning that pushed him to address risk factors before they became a crisis.
What to ask your clinician (a short list)
- Could my ED be related to blood pressure, lipids, or blood sugar?
- Do I have risk factors that warrant deeper evaluation (family history, diabetes, smoking history, symptoms with exertion)?
- Are any of my medications contributing (certain blood pressure meds, antidepressants, etc.)?
- Is testosterone relevant here, and if so, what’s the right way to measure and interpret it?
- If considering a PDE5 inhibitor, what are the safety rules (including nitrate interactions) and what is the appropriate dosing strategy?
Common pitfalls
- Treating ED as purely psychological without assessing cardiometabolic risk—especially after 40.
- Chasing quick fixes while ignoring sleep, daily movement, and nutrition quality.
- Overtraining (high intensity every day) while under-recovering, which can worsen stress physiology.
- Using online supplements or hormones without medical oversight or proper lab interpretation.
- Ignoring safety: PDE5 inhibitors can be dangerous with nitrate medications—this must be discussed with a clinician.
Practical next steps
- Treat symptoms as signals: ask for a cardiovascular and metabolic risk review alongside sexual health discussion.
- Start with the basics for 30 days: Zone 2, two strength sessions weekly, and a consistent sleep schedule.
- Eat for vessel health: more fiber and minimally processed foods; add nitrate-rich vegetables regularly.
- Track blood pressure at home if recommended, and bring trends—not guesses—to appointments.
- If you have chest pain, shortness of breath with exertion, fainting, or severe symptoms, seek prompt medical evaluation.
Quick checklist
- Blood pressure is monitored (trend known).
- Sleep averages close to 7 hours when possible, with a consistent wake time.
- Training includes both aerobic base (Zone 2) and strength work.
- Meals include protein + fiber most days; ultra-processed intake is reduced.
- A clinician has reviewed medications and cardiometabolic risk factors.
Important note: This article is educational and not medical advice. Erectile dysfunction has many causes, and any treatment should be individualized with a qualified clinician. If you have concerning symptoms (chest pain, severe shortness of breath, fainting, or signs of cardiovascular disease), seek medical care promptly. Never mix ED medications with nitrates unless explicitly cleared by a clinician.